Pregnancy SmartSiteTM
Seizure disorder - children; Convulsion - childhood epilepsy; Medically refractory childhood epilepsy; Anticonvulsant - childhood epilepsy; Antiepileptic drug - childhood epilepsy; AED - childhood epilepsy DefinitionEpilepsy is a brain disorder in which a person has repeated seizures over time. A seizure is a sudden change in the electrical and chemical activity in the brain. A single seizure that does not happen again is not epilepsy. CausesEpilepsy may be due to a medical condition or injury that affects the brain. Or the cause may be unknown. Common causes of epilepsy include:
Epileptic seizures usually start between ages 5 and 20. But they can happen at any age. There may be a family history of seizures or epilepsy. A febrile seizure is a convulsion in a child triggered by a fever. Most of the time, a febrile seizure is not a sign that the child has epilepsy. SymptomsSymptoms vary from child to child. Some children may simply stare. Others may shake violently and lose alertness. The movements or symptoms of a seizure may depend on the part of the brain that is affected. Your child's health care provider can tell you more about the specific type of seizure your child may have:
Some children can have more than one type of seizure. Most of the time, the seizure is similar to the one before it, although that may change over time. Some children have a strange sensation before a seizure. Sensations may be tingling, smelling an odor that is not actually there, feeling fear or anxiety for no reason or having a sense of déjà vu (feeling that something has happened before). This is called an aura. Exams and TestsThe provider will:
Your child's provider may order an electroencephalogram (EEG) to check the electrical activity in the brain. This test often shows any abnormal electrical activity in the brain. In some cases, the test shows the area in the brain where the seizures start. The brain may appear normal after a seizure or between seizures. To diagnose epilepsy or plan for epilepsy surgery, your child may need to:
Your child's provider also may order other tests, including:
Head CT or MRI scan are often done to find the cause and location of the problem in the brain. Much less often, PET scan of the brain is needed to help plan surgery. TreatmentTreatment for epilepsy includes:
If your child's epilepsy is due to a tumor, abnormal blood vessels, or bleeding in the brain, surgery may be needed. Medicines to prevent seizures are called antiseizure medicines. They are also known as anticonvulsants or antiepileptic medicines. These may reduce the number of future seizures.
Other medicines are used to stop a seizure that doesn't stop on its own. These can be given under the tongue or by an injection into the muscle. They are called rescue medicines. Many antiseizure medicines may affect your child's bone health. Talk to your child's provider about whether your child needs vitamins and other supplements. Epilepsy that is not well controlled after trying a number of antiseizure medicines is called medically refractory epilepsy. In this case, your child's provider may recommend surgery to:
Some children are placed on a special diet to help prevent seizures. The most popular one is the ketogenic diet. A diet low in carbohydrates, such as the Atkins diet, also may be helpful. Be sure to discuss these options with your child's provider before trying them. Epilepsy is often a lifelong or chronic illness. Important management issues include:
Managing these lifestyle or medical issues at home can be a challenge. Be sure to talk with your child's provider if you have concerns. Support GroupsThe stress of being a caretaker of a child with epilepsy can often be helped by joining a support group. In these groups, members share common experiences and problems. Outlook (Prognosis)Most children with epilepsy live a normal life. Certain types of childhood epilepsy go away or improve with age, usually in the late teens or 20s. If your child does not have seizures for a few years, your provider may suggest stopping their medicines. For many children, epilepsy is a lifelong condition. In these cases, the medicines need to be continued. Children who have developmental disorders in addition to epilepsy may face challenges throughout their life. Knowing more about the condition will help you take better care of your child's epilepsy. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalCall 911 or the local emergency number if:
If your child has had seizures before, call 911 or the local emergency number for any of these emergency situations:
Contact your child's provider if your child has new symptoms:
Contact your child's provider even if your child is normal after the seizure has stopped. PreventionThere is no known way to prevent epilepsy. Proper diet and sleep may decrease the chances of seizures in children with epilepsy. Reduce the risk of head injury during risky activities by wearing a helmet. This can decrease the likelihood of a brain injury that leads to seizures and epilepsy. ReferencesGhatan S. Pediatric epilepsy surgery. In: Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 267. Kanner AM, Ashman E, Gloss D, et al. Practice guideline update summary: efficacy and tolerability of the new antiepileptic drugs I: treatment of new-onset epilepsy: report of the American Epilepsy Society and the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Epilepsy Curr. 2018;18(4):260-268. PMID: 30254527 pubmed.ncbi.nlm.nih.gov/30254527/. Mikati MA, Tchapyjnikov D, Rathke KM. Seizures in childhood. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 633. Pearl PL. Overview of seizures and epilepsy in children. In: Swaiman KF, Ashwal S, Ferriero DM, et al, eds. Swaiman's Pediatric Neurology: Principles and Practice. 6th ed. Philadelphia, PA: Elsevier; 2017:chap 61. | ||
| ||
Review Date: 6/13/2024 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


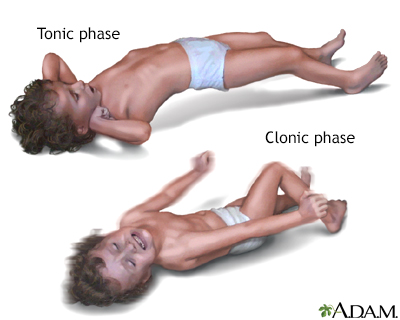 Grand mal seizure
Grand mal seizure
