Pregnancy SmartSiteTM
Human papilloma virus - testing; Abnormal Pap smear - HPV testing; LSIL-HPV testing; Low-grade dysplasia - HPV testing; HSIL - HPV testing; High-grade dysplasia - HPV testing; HPV testing in women; Cervical cancer - HPV DNA test; Cancer of cervix - HPV DNA test DefinitionThe HPV test is used to check for infection with HPV types associated with cervical cancer. Typically, the test looks for 14 different HPV types. HPV type 16 and HPV type 18 are most closely associated with cervical cancer. How the Test Is PerformedThe HPV test may be done during a Pap test. If they are done together, it is called "co-testing." You lie on a table and place your feet in footrests. Your health care provider inserts an instrument (called a speculum) into the vagina to open it slightly. This allows the provider to see the cervix. Cells are gently collected from the cervix area. The cervix is the lower part of the womb (uterus) that opens at the top of the vagina. The sample of cells is sent to a lab for examination. How to Prepare for the TestNo special preparation is required for an HPV test. If you're getting a Pap test at the same time, it is recommended that you do NOT do the following in the 24 hours before the test:
For your comfort, you may want to empty your bladder just before the test. How the Test will FeelThe exam may cause some discomfort. Some people say it feels like menstrual cramps. You may also feel some pressure during the exam. You may bleed a bit after the test. Why the Test Is PerformedHigh-risk types of HPV can lead to cervical cancer. The HPV test is done to determine if you are infected with one of these high-risk types. Your provider may order an HPV test:
The HPV test results help your provider decide if further testing or treatment is needed. Normal ResultsA normal result means you do not have a high-risk type of HPV. You may be asked to return in 3 or 5 years for repeat testing. What Abnormal Results MeanAn abnormal result means you have one or more high-risk types of HPV. If HPV types 16 or 18 are detected, your provider will likely recommend colposcopy. This is a procedure in which the cervix is magnified with a binocular-like instrument. Small biopsies (tissue samples) are often taken during this procedure to look for evidence of a precancerous change or cancer. If the test is positive for one or more of the other high-risk HPV types, repeat testing in one year may be recommended. Your provider will advise you about next steps if your test is positive. ReferencesFontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020 Sep;70(5):321-346. Epub 2020 Jul 30. PMID: 32729638 pubmed.ncbi.nlm.nih.gov/32729638/. Perkins RB, Guido RS, Castle PE, et al. 2019 ASCCP Risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2020;24(2):102-131. PMID: 32243307 pubmed.ncbi.nlm.nih.gov/32243307/. Salcedo MP, Phoolcharoen N, Schmeler KM. Intraepithelial neoplasia of the lower genital tract (cervix, vagina, vulva): Etiology, screening, diagnosis, management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 29. US Preventive Services Task Force website. Cervical cancer: Screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screening. Updated August 21, 2018. Accessed January 28, 2025. Wang ZX, Peiper SC. HPV detection techniques. In: Bibbo M, Wilbur DC, eds. Comprehensive Cytopathology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 38. | ||
| ||
Review Date: 10/15/2024 Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


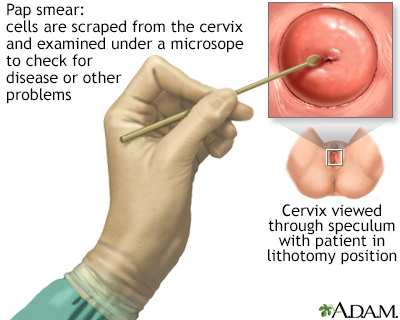 Pap smear
Pap smear
