Pregnancy SmartSiteTM
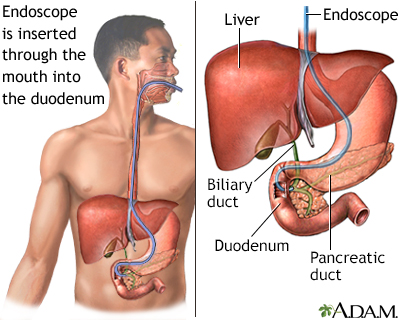
Endoscopic retrograde cholangiopancreatography DefinitionERCP is short for endoscopic retrograde cholangiopancreatography. It is a procedure that looks at the bile and pancreatic ducts. It is done through an endoscope.
DescriptionAn intravenous (IV) line is placed in your arm. You will lie on your stomach or on your left side for the test.
After the sedative takes effect, the endoscope is inserted through the mouth. It goes through the esophagus (food pipe) and stomach until it reaches the duodenum (the part of the small intestine that is closest to the stomach).
A thin tube (catheter) is passed through the endoscope and inserted into the tubes (ducts) that lead to the pancreas and gallbladder. A special dye is injected into these ducts, and x-rays are taken. This helps the doctor see stones, tumors, and any areas that have become narrowed. Special instruments can be placed through the endoscope and into the ducts. Why the Procedure Is PerformedThe procedure is used mostly to treat or diagnose problems of the pancreas or bile ducts that can cause abdominal pain (most often in the right upper or middle stomach area) and yellowing of the skin and eyes (jaundice). ERCP may be used to:
Note: Imaging tests generally will be done to diagnose the cause of symptoms before an ERCP is done. These include ultrasound tests, CT scan, or MRI scan. RisksRisks of the procedure include:
Before the ProcedureYou will need to not eat or drink for at least 4 hours before the test. You will sign a consent form. Remove all jewelry so that it will not interfere with the x-ray. Tell your health care provider if you have allergies to iodine or you have had reactions to other dyes used to take x-rays. You will need to arrange a ride home after the procedure. After the ProcedureSomeone will need to drive you home from the hospital. The air that is used to inflate the stomach and bowel during an ERCP procedure can cause some bloating or gas for about 24 hours. After the procedure, you may have a sore throat for the first day. Soreness may last for up to 3 to 4 days. Do only light activity on the first day after the procedure. Avoid heavy lifting for the first 48 hours. You can treat pain with acetaminophen (Tylenol). DO NOT take aspirin, ibuprofen, or naproxen. Putting a heating pad on your belly may relieve pain and bloating. The provider will tell you what to eat. Most often, you will want to drink fluids and eat only a light meal on the day after the procedure. Contact your provider if you have:
ReferencesFogel EL, Sherman S. Diseases of the gallbladder and bile ducts. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 141. James TW, Baron TH. Endoscopic and radiologic treatment of biliary disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 70. Khan S, Singh VK. Obstructive jaundice: the role of endoscopic intervention. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:532-538. Lidofsky SD. Jaundice. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 21. | ||
| ||
Review Date: 4/21/2025 Reviewed By: Todd Eisner, MD, Private practice specializing in Gastroenterology in Boca Raton and Delray Beach, Florida at Gastroenterology Consultants of Boca Raton. Affiliate Assistant Professor, Florida Atlantic University School of Medicine. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 ERCP
ERCP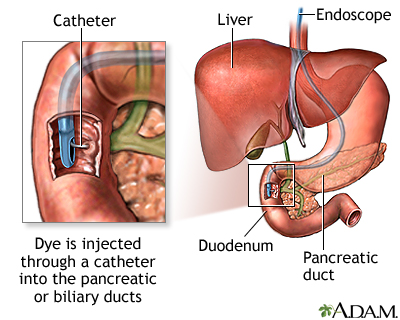 ERCP
ERCP
