Pregnancy SmartSiteTM
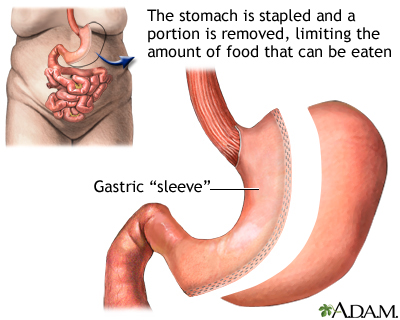
Gastrectomy - sleeve; Gastrectomy - greater curvature; Gastrectomy - parietal; Gastric reduction; Vertical gastroplasty DefinitionVertical sleeve gastrectomy is surgery to help with weight loss. The surgeon removes a large portion of your stomach. The new, smaller stomach is about the size of a banana. It limits the amount of food you can eat and makes you feel full after eating small amounts of food. DescriptionYou will receive general anesthesia before this surgery. This is medicine that keeps you asleep and pain-free. The surgery is usually done using a small camera that is placed in your belly. This type of surgery is called laparoscopy. The camera is called a laparoscope. It allows your surgeon to see inside your belly. In this surgery:
The surgery takes 60 to 90 minutes. Weight-loss surgery may increase your risk for gallstones. Your surgeon may recommend having a cholecystectomy. This is surgery to remove the gallbladder. It may be done before the weight-loss surgery or at the same time. Why the Procedure Is PerformedWeight-loss surgery may be an option if you are very obese and have not been able to lose weight through diet and exercise. Vertical sleeve gastrectomy is not a quick fix for obesity. It will greatly change your lifestyle. After this surgery, you must eat healthy foods, control portion sizes of what you eat, and exercise. If you do not follow these measures, you may have complications from the surgery and poor weight loss. This procedure may be recommended if you have:
Vertical sleeve gastrectomy has most often been done on people who are too heavy to safely have other types of weight-loss surgery. Some people may eventually need a second weight-loss surgery. This procedure cannot be reversed once it has been done. RisksRisks for anesthesia and surgery in general are:
Risks for vertical sleeve gastrectomy are:
Before the ProcedureYour surgeon will ask you to have tests and visits with your other health care providers before you have this surgery. Some of these are:
Tell your surgeon or nurse:
Planning for your surgery:
During the week before your surgery:
On the day of your surgery:
After the ProcedureYou can usually go home 2 days after your surgery. You should be able to drink clear liquids on the day after surgery, and then go on a pureed diet by the time you go home. When you go home, you will probably be given pain pills or liquids and a medicine called a proton pump inhibitor, which reduces the amount of acid in your stomach. When you eat after having this surgery, the small pouch will fill quickly. You will feel full after eating a very small amount of food. Your surgeon, nurse, or dietitian will recommend a diet for you. Meals should be small to avoid stretching the remaining stomach. When you go home, you should plan to get up and walk a few times a day and increase your activity as tolerated. Outlook (Prognosis)The final weight loss may not be as large as with gastric bypass. This may be enough for many people. Talk with your surgeon about which procedure is best for you. The weight will usually come off more slowly than with gastric bypass. You should keep losing weight for up to 2 to 3 years. Losing enough weight after surgery can improve many medical conditions you might also have. Conditions that may improve are asthma, type 2 diabetes, arthritis, high blood pressure, obstructive sleep apnea, high cholesterol, and gastroesophageal disease (GERD). Weighing less should also make it much easier for you to move around and do your everyday activities. This surgery alone is not a solution to losing weight. It can train you to eat less, but you still have to do much of the work. To lose weight and avoid complications from the procedure, you will need to follow the exercise and eating guidelines that your surgeon and dietitian give you. ReferencesAmerican Society for Metabolic and Bariatric Surgery website. Bariatric surgery procedures. asmbs.org/patients/bariatric-surgery-procedures. Updated May 2021. Accessed January 27, 2025. Richards WO, Khaitan L, Torquati A. Morbid obesity. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 48. Sullivan S, Edmundowicz SA, Morton JM. Surgical and endoscopic treatment of obesity. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 8. | ||
| ||
Review Date: 1/21/2025 Reviewed By: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Gastric sleeve pro...
Gastric sleeve pro...
