Pregnancy SmartSiteTM
PFTs; Spirometry; Spirogram; Lung function tests; Lung volume; Plethysmography DefinitionPulmonary function tests are a group of tests that measure breathing and how well the lungs are functioning. How the Test is PerformedSpirometry measures airflow. By measuring how much air you exhale, and how quickly you exhale, spirometry can evaluate a broad range of lung diseases. In a spirometry test, while you are sitting, you breathe into a mouthpiece that is connected to an instrument called a spirometer. The spirometer records the amount and the rate of air that you breathe in and out over a period of time. When standing, some numbers might be slightly different. For some of the test measurements, you can breathe normally and quietly. Other tests require forced inhalation or exhalation after a deep breath. Sometimes, you will be asked to inhale a different gas or a medicine to see how it changes your test results. Lung volume measurement can be done in two ways:
To measure diffusion capacity, you breathe a harmless gas, called a tracer gas, for a very short time, often for only one breath. The concentration of the gas in the air you breathe out is measured. The difference in the amount of gas inhaled and exhaled measures how effectively gas travels from the lungs into the blood. This test allows your health care provider to estimate how well your lungs move oxygen from the air into your bloodstream. How to Prepare for the TestDo not eat a heavy meal before the test. Do not smoke for 4 to 6 hours before the test. You will get specific instructions if you need to stop using bronchodilators or other inhaled medicines. You may have to breathe in medicine before or during the test. How the Test will FeelSince the test involves some forced breathing and rapid breathing, you may have some temporary shortness of breath or lightheadedness. You also might have some coughing. You breathe through a tight-fitting mouthpiece and you will have nose clips. If you are claustrophobic, the part of the test in the closed booth may feel uncomfortable. Follow instructions for using the mouthpiece of the spirometer. A poor seal around the mouthpiece may cause results that aren't accurate. Why the Test is PerformedPulmonary function tests are done to:
Normal ResultsPredicted results that compare you to your peers in age, sex, height and weight are utilized and your results are calculated to be a percentage of these. Your results are considered abnormal if they are significantly lower. Normal value ranges may vary slightly among different laboratories, based on slightly different ways to determine normal values. Talk to your provider about the meaning of your specific test results. Different measurements that may be found on your report after pulmonary function tests commonly include:
What Abnormal Results MeanAbnormal results usually mean that you may have chest or lung disease. Some lung diseases (such as emphysema, asthma, chronic bronchitis, and infections) mainly affect the airways that carry air to and from the lungs. They can make the lungs contain too much air and take longer to empty. These lung diseases are called obstructive lung disorders. Other lung diseases make the lungs scarred and smaller so that they contain too little air and are poor at transferring oxygen into the blood. Examples of these types of illnesses include:
Muscular weakness can also cause abnormal test results, even if the lungs are normal, that is, similar to the diseases that cause smaller lungs. RisksThere is a small risk for collapsed lung (pneumothorax) in people with a certain type of lung disease. The test should not be given to a person who has experienced a recent heart attack, has certain other types of heart disease, or has had a recent collapsed lung. ReferencesBhakta NR, Kaminsky DA. Pulmonary function testing: physiologic and testing principles. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 31. Scanlon PD, Niven AS. Respiratory testing and function. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 73. Wald O, Izhar U, Sugarbaker DJ. Lung, chest wall, pleura, and mediastinum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 58. | ||
| ||
Review Date: 11/25/2023 Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 02/05/2025. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


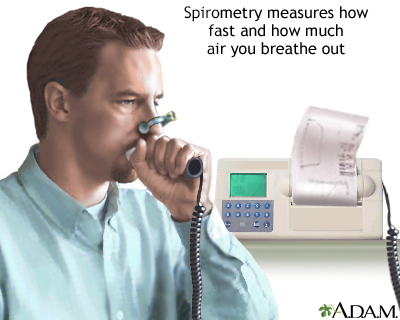 Spirometry
Spirometry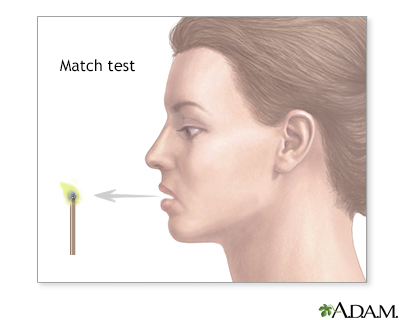 Match test
Match test
