Pregnancy SmartSiteTM
Purified protein derivative standard; TB skin test; Tuberculin skin test; Mantoux test DefinitionThe PPD skin test is a method used to diagnose silent (latent) tuberculosis (TB) infection. PPD stands for purified protein derivative. How the Test is PerformedYou will need two visits to your health care provider's office for this test. At the first visit, the provider will clean an area of your skin, usually the inside of your forearm. You will get a small shot (injection) that contains PPD. The needle is gently placed under the top layer of skin, causing a bump (welt) to form. This bump usually goes away in a few hours as the material is absorbed. After 48 to 72 hours, you must return to your provider's office (in some cases, this can be done virtually). Your provider will check the area to see if you have had a strong reaction to the test. How to Prepare for the TestThere is no special preparation for this test. Tell your provider if you have ever had a positive PPD skin test. If so, you should not have a repeat PPD test, except under unusual circumstances. Tell your provider if you have a medical condition or if you take certain medicines, such as steroids, which can affect your immune system. These situations may lead to inaccurate test results. Tell your provider if you have received the BCG vaccine and if so, when you received it. (This vaccine is only given outside of the United States). How the Test will FeelYou will feel a brief sting as the needle is inserted just below the skin surface. Why the Test is PerformedThis test is done to find out if you have ever come in contact with the bacteria that cause TB. TB is an easily spread (contagious) disease. It most often affects the lungs. The bacteria can remain inactive (dormant) in the lungs for many years. This situation is called latent TB. Most people in the United States who are infected with the bacteria do not have signs or symptoms of active TB. You are most likely to need this test if you:
Normal ResultsA negative reaction usually means you have never been infected with the bacteria that cause TB. With a negative reaction, the skin where you received the PPD test is not swollen, or the swelling is very small. Interpreting the size of the swelling is different for children, people with HIV, and other high-risk groups. The PPD skin test is not a perfect screening test. A few people infected with the bacteria that cause TB may not have a reaction. Also, diseases or medicines that weaken the immune system may cause a false-negative result. What Abnormal Results MeanAn abnormal (positive) result means you have been infected with the bacteria that cause TB. You may need treatment to lower the risk of the disease coming back (reactivation of the disease). A positive skin test does not mean that a person has active TB. More tests must be done to check whether there is active disease. A small reaction (5 mm or more of firm swelling at the site) is considered to be positive in people:
Larger reactions (10 mm or more) are considered positive in:
In people with no known risks of TB, 15 mm or more of firm swelling at the site indicates a positive reaction. People who were born outside the United States who have had a vaccine called BCG may have a false-positive test result. RisksThere is a very small risk for severe redness and swelling of the arm in people who have had a previous positive PPD test and who have the test again. Generally, people who have had a positive test in the past should not be retested. This reaction can also occur in a few people who have not been tested before. ReferencesCenters for Disease Control and Prevention website. Tuberculosis (TB). About tuberculosis. www.cdc.gov/tb/about/index.html. Reviewed December 19, 2023. Accessed June 25, 2024. Fitzgerald DW, Sterling TR, Haas DW. Mycobacterium tuberculosis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 249. Rodino KG, Woods GL, Wengenack NL. Mycobacteria. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 59. | ||
| ||
Review Date: 12/31/2023 Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 06/25/2024. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


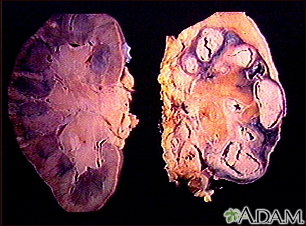 Tuberculosis in th...
Tuberculosis in th...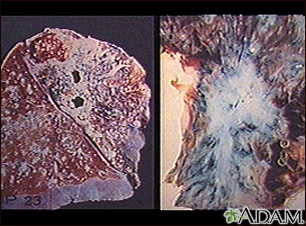 Tuberculosis in th...
Tuberculosis in th... Positive PPD skin ...
Positive PPD skin ...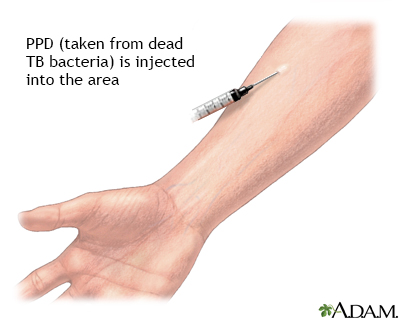 PPD skin test
PPD skin test
