Pregnancy SmartSiteTM
Pyrosis; GERD (gastroesophageal reflux disease); Esophagitis DefinitionHeartburn is a painful burning feeling just below or behind the breastbone. Most of the time, it comes from the esophagus. The pain often rises in your chest from your stomach. It may also spread to your neck or throat. CausesAlmost everyone has heartburn at some time. If you have heartburn very often, you may have gastroesophageal reflux disease (GERD). Normally when food or liquid enters your stomach, a band of muscle at the lower end of your esophagus closes off the esophagus. This band is called the lower esophageal sphincter (LES). If this band does not close tightly enough, food or stomach acid can back up (reflux) into the esophagus. The stomach contents can irritate the esophagus and cause heartburn and other symptoms. Heartburn is more likely if you have a hiatal hernia. A hiatal hernia is a condition which occurs when the top part of the stomach pokes into the chest cavity. This weakens the LES so that it is easier for acid to back up from the stomach into the esophagus. Pregnancy and many medicines can bring on heartburn or make it worse. Medicines that can cause heartburn include:
Talk to your health care provider if you think one of your medicines may be causing heartburn. Never change or stop taking medicine without talking to your provider first. Home CareYou should treat frequent heartburn (heartburn that occurs 2 or more days per week) because reflux can damage the lining of your esophagus. This can cause serious problems over time. Changing your habits can be helpful in preventing heartburn and other symptoms of GERD. The following tips will help you avoid heartburn and other GERD symptoms. Talk to your provider if you are still bothered by heartburn after trying these steps. First, avoid foods and drinks that can trigger reflux, such as:
Next, try changing your eating habits:
Make other lifestyle changes as needed:
If you still do not have full relief, try over-the-counter medicines:
When to Contact a Medical ProfessionalGet urgent medical care if:
Contact your provider if:
What to Expect at Your Office VisitHeartburn is easy to diagnose from your symptoms in most cases. Sometimes, heartburn can be confused with another stomach problem called dyspepsia. If the diagnosis is unclear, you may be referred to a doctor called a gastroenterologist for more testing. First, your provider will do a physical exam and ask questions about your heartburn, such as:
Your provider may suggest one or more of the following tests:
If your symptoms do not get better with home care, you may need to take medicine to reduce acid that is stronger than over-the-counter medicines. Any sign of bleeding will need more testing and treatment. ReferencesChang L. Irritable bowel and functional upper gastrointestinal syndromes. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 123. DeVault KR. Symptoms of esophageal disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 13. Falk GW, Katzka DA. Diseases of the esophagus. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 124. | ||
| ||
Review Date: 1/24/2025 Reviewed By: Jenifer K. Lehrer, MD, Gastroenterologist, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


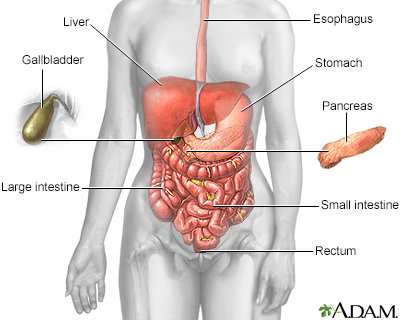 Digestive system
Digestive system Hiatal hernia - X-...
Hiatal hernia - X-...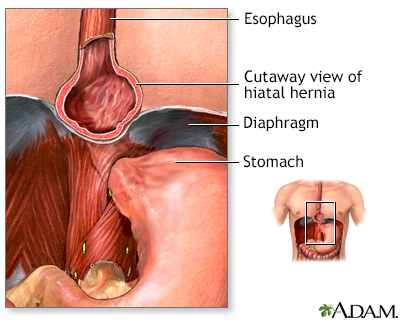 Hiatal hernia
Hiatal hernia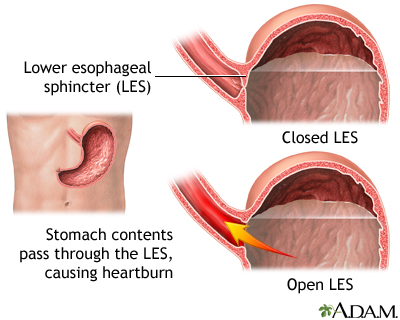 Gastroesophageal r...
Gastroesophageal r...
