Pregnancy SmartSiteTM
Repair of cross-eye; Resection and recession; Strabismus repair; Extraocular muscle surgery DefinitionEye muscle repair is surgery to correct eye muscle problems that cause strabismus (crossed eyes). DescriptionThe goal of this surgery is to restore the eye muscles to a proper position. This will help the eyes move correctly. Eye muscle surgery is most often done on children. However, adults who have similar eye problems may also have it done. Children will most often have general anesthesia for the procedure. They will be asleep and will not feel pain. Depending on the problem, one or both eyes may need surgery. After the anesthesia has taken effect, the eye surgeon makes a small surgical cut in the clear tissue covering the white of the eye. This tissue is called the conjunctiva. Then the surgeon will locate one or more of the eye muscles that needs surgery. Sometimes the surgery strengthens the muscle, and sometimes it weakens it.
The surgery for adults is similar. In most cases, adults are awake, but are given medicine to numb the area and help them relax. When the procedure is done on adults, an adjustable stitch is used on the weakened muscle so that minor changes can be made later that day or the next day. This technique often has a very good outcome. Why the Procedure Is PerformedStrabismus is a disorder in which the two eyes do not line up in the same direction. Therefore, the eyes do not focus on the same object at the same time. The condition is more commonly known as "crossed eyes." Surgery may be recommended when strabismus does not improve with glasses or eye exercises. RisksRisks for any anesthesia are:
Risks for any surgery are:
Some risks for this surgery include:
Before the ProcedureYour child's eye surgeon may ask for:
Always tell your child's health care provider:
During the days before the surgery:
On the day of the surgery:
After the ProcedureMost of the time, the surgery does not need an overnight stay in the hospital. The eyes are most often straight right after surgery. While recovering from the anesthesia and in the first few days after surgery, your child should avoid rubbing their eyes. Your surgeon will show you how to prevent your child from rubbing their eyes. After a few hours of recovery, your child may go home. You should have a follow-up visit with the eye surgeon 1 to 2 weeks after the surgery. To prevent infection, you will probably need to put drops or ointment in your child's eyes. Outlook (Prognosis)Eye muscle surgery does not fix the poor vision of a lazy (amblyopic) eye. Your child may have to wear glasses or a patch. In general, the younger a child is when the operation is performed, the better the result. Your child's eyes should look normal a few weeks after the surgery. ReferencesCoats DK, Olitsky SE. Strabismus surgery. In: Lyons CJ, Lambert SR, eds. Taylor and Hoyt's Pediatric Ophthalmology and Strabismus. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 88. Feuillade V, Bourcier T, Gaucher D, Speeg C, Sauer A. The effect of strabismus surgery on the learning abilities of school-aged children. Acta Ophthalmol. 2023:101(5):546-552. PMID: 36691981 pubmed.ncbi.nlm.nih.gov/36691981/. Heidary G, Aakalu VK, Binenbaum G, et al. Adjustable sutures in the treatment of strabismus: a report by the American Academy of Ophthalmology. Ophthalmology. 2022;129(1):100-109. PMID: 34446304 pubmed.ncbi.nlm.nih.gov/34446304/. Olitsky SE, Marsh JD. Disorders of eye movement and alignment. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 663. Robbins SL. Techniques of strabismus surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 11.13. | ||
| ||
Review Date: 8/5/2024 Reviewed By: Franklin W. Lusby, MD, Ophthalmologist, Lusby Vision Institute, La Jolla, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


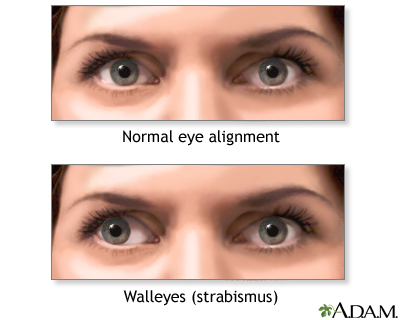 Walleyes
Walleyes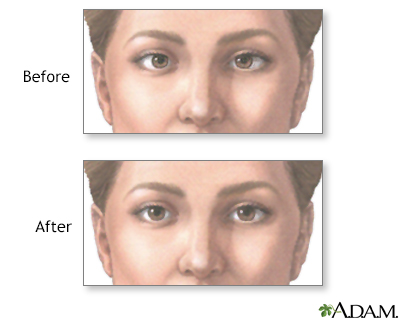 Before and after s...
Before and after s...
