Pregnancy SmartSiteTM
Scleral buckling; Vitrectomy; Pneumatic retinopexy; Laser retinopexy; Rhegmatogenous retinal detachment repair DefinitionRetinal detachment repair is eye surgery to place a retina back into its normal position. The retina is the light-sensitive tissue in the back of the eye. Detachment means that it has pulled away from the layers of tissue around it. This article describes the repair of rhegmatogenous retinal detachments. These occur due to a hole or tear in the retina. DescriptionMost retinal detachment repair operations are urgent. If holes or tears in the retina are found before the retina detaches, the eye doctor can close the holes using a laser. This procedure is most often done in the eye doctor's office. In any surgery to repair a retinal detachment there are two steps. In one step, a scar around the tear or hole is created usually using a cryoprobe or a laser. The other step is to "push" the separated layers of the retina back together. There are two ways: push them together from the inside using a gas bubble inside the eye (retinopexy) or push them together from the outside using a scleral buckle. The type of detachment (size, location) will determine which step occurs first. If the retina has just started to detach, a procedure called pneumatic retinopexy may be done to repair it.
Severe detachments need more advanced surgery. The following procedures are done in a hospital or outpatient surgery center:
In complex cases, both procedures may be done at the same time. Why the Procedure Is PerformedRetinal detachments do not get better without treatment. Repair is needed to prevent permanent vision loss. How quickly the surgery needs to be done depends on the location and extent of the detachment. If possible, the surgery should be done the same day if the detachment has not affected the central vision area (the macula). This can help prevent further detachment of the retina. It also will increase the chance of preserving good vision. If the macula detaches, it is too late to restore normal vision. Surgery can still be done to prevent total blindness. In these cases, eye doctors can wait a week to 10 days to schedule surgery. RisksRisks for retinal detachment surgery include:
General anesthesia may be needed. The risks for any anesthesia are:
You may not recover full vision. After the ProcedureThe chances of successful reattachment of the retina depend on the number of holes, their size, and whether there is scar tissue in the area. In most cases, the procedures do not require an overnight hospital stay. You may need to limit your physical activity for some time. If the retina is repaired using the gas bubble procedure, you need to keep your head face down or turned to one side for several days or weeks. It is important to maintain this position so the gas bubble pushes the retina into place. People with a gas bubble in the eye may not fly or go to high altitudes until the gas bubble dissolves. This most often happens within a few weeks. Outlook (Prognosis)Most of the time, the retina can be reattached with one operation. However, some people will need several surgeries. More than 9 out of 10 detachments can be repaired. Failure to repair the retina always results in loss of vision to some degree. When a detachment occurs, the photoreceptors (rods and cones) start to degenerate. The sooner the detachment is repaired, the sooner the retina will begin to recover. However, once the retina has detached, its rods and cones that detect light (the photoreceptors) may never recover completely. After surgery, the quality of vision depends on where the detachment occurred, and the cause:
ReferencesCioffi GA, Liebmann JM. Diseases of the visual system. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 391. Guluma K, Lee JE. Ophthalmology. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 57. Todorich B, Faia LJ, Williams GA. Scleral buckling surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 6.9. Wickham L, Aylward GW. Optimal procedures for retinal detachment repair. In: Sadda SVR, Sarraf D, Freund KB, et al, eds. Ryan's Retina. 7th ed. Philadelphia, PA: Elsevier; 2023:chap 108. | ||
| ||
Review Date: 8/5/2024 Reviewed By: Franklin W. Lusby, MD, Ophthalmologist, Lusby Vision Institute, La Jolla, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


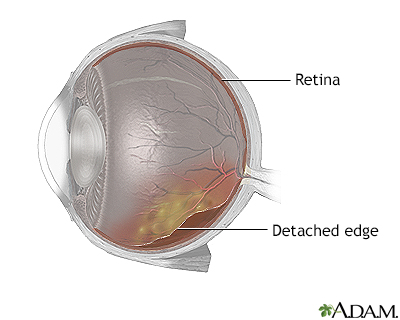 Detached retina
Detached retina
