Pregnancy SmartSiteTM
Renal disease - diet; Kidney disease - diet DefinitionYou may need to make changes to your diet when you have chronic kidney disease (CKD). These changes may include limiting fluids, eating a low-protein diet, limiting salt, potassium, phosphorous, and other electrolytes, and getting enough calories if you are losing weight. You may need to alter your diet more if your kidney disease gets worse, or if you need dialysis. FunctionThe purpose of this diet is to keep the levels of electrolytes, minerals, and fluid in your body balanced when you have CKD or are on dialysis. People on dialysis need this special diet to limit the buildup of waste products in the body. Limiting fluid intake between dialysis treatments is very important because most people on dialysis urinate very little. Without urination, fluid will build up in the body and cause too much fluid in the heart and lungs. RecommendationsAsk your health care provider to refer you to a registered dietitian to help you with your diet for kidney disease. Some dietitians specialize in kidney diets. Your dietitian can also help you create a diet to fit your other health needs. The Kidney Foundation has chapters in most states. It is a good place for people with kidney disease and their families to find programs and information. You need to take in enough calories each day to keep you healthy and prevent the breakdown of body tissue. Ask your provider and dietitian what your ideal weight should be. Weigh yourself every morning to make sure you are meeting this goal. CARBOHYDRATES If you do not have a problem eating carbohydrates, these foods are a good source of energy. If your provider has recommended a low-protein diet, you may replace the calories from protein with:
FATS Fats can be a good source of calories. Make sure to use monounsaturated and polyunsaturated fats (olive oil, canola oil, safflower oil) to protect your heart health. Talk to your provider or dietitian about fats and cholesterol that may increase your risk for heart problems. PROTEIN Low-protein diets may be helpful before you start dialysis. Your provider or dietitian may advise a lower-protein diet based on your weight, stage of disease, how much muscle you have, and other factors. But you still need enough protein, so work with your provider to find the right diet for you. Once you start dialysis, you will need to eat more protein. A high-protein diet with fish, poultry, pork, or eggs at every meal may be recommended. People on dialysis should eat 8 to 10 ounces (225 to 280 grams) of high-protein foods each day. Your provider or dietitian may suggest adding egg whites, egg white powder, or protein powder. CALCIUM AND PHOSPHOROUS The minerals calcium and phosphorous will be checked often. Even in the early stages of CKD, phosphorous levels in the blood can get too high. This can cause:
You will need to limit the amount of dairy foods you eat, because they contain large amounts of phosphorous. This includes milk, yogurt, and cheese. Some dairy foods are lower in phosphorous, including:
You may need to take calcium supplements to prevent bone disease, and vitamin D to control the balance of calcium and phosphorous in your body. Ask your provider or dietitian about how best to get these nutrients. Your provider may recommend medicines called "phosphorous binders" if diet changes alone do not work to control the balance of this mineral in your body. FLUIDS In the early stages of kidney failure, you do not need to limit the fluid you drink. But, as your condition gets worse, or when you are on dialysis, you will need to watch the amount of liquid you take in. In between dialysis sessions, fluid can build up in your body. Too much fluid will lead to shortness of breath, an emergency that needs immediate medical attention. Your provider and dialysis nurse will let you know how much you should drink every day. Keep a count of foods that contain a lot of water, such as soups, fruit-flavored gelatin, fruit-flavored ice pops, ice cream, grapes, melons, lettuce, tomatoes, and celery. Use smaller cups or glasses and turn over your cup after you have finished it. Tips to keep from becoming thirsty include:
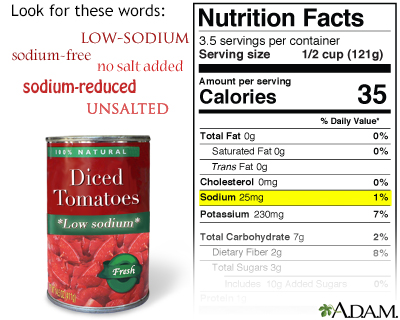
SALT OR SODIUM Reducing sodium in your diet helps you control high blood pressure. It also keeps you from being thirsty, and prevents your body from holding onto extra fluid. Look for these words on food labels:
Check all labels to see how much salt or sodium foods contain per serving. Also, avoid foods that list salt near the beginning of the ingredients. Look for products with less than 100 milligrams (mg) of salt per serving. DO NOT use salt when cooking and take the salt shaker away from the table. Most other herbs are safe, and you can use them to flavor your food instead of salt. DO NOT use salt substitutes because they contain potassium. People with CKD also need to limit their potassium. POTASSIUM Normal blood levels of potassium help keep your heart beating steadily. However, too much potassium can build up when the kidneys no longer function well. Dangerous heart rhythms may result, which can lead to death. Fruits and vegetables contain large amounts of potassium, and for that reason should be limited to maintain a healthy heart. Choosing the right item from each food group can help control your potassium levels. When eating fruits:
When eating vegetables:
IRON People with advanced kidney failure also have anemia and usually need extra iron. Many foods contain extra iron (liver, beef, pork, chicken, lima and kidney beans, iron-fortified cereals). Talk to your provider or dietitian about which foods with iron you can eat because of your kidney disease. ReferencesGoraya N, Wesson DE. Dietary approaches to kidney diseases. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 60. Levey AS, Sarnak MJ. Chronic kidney disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 116. National Institute of Diabetes and Digestive and Kidney Diseases website. Eating & nutrition for hemodialysis. www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis/eating-nutrition. Updated September 2016. Accessed September 8, 2023. National Kidney Foundation website. Dietary guidelines for adults starting on hemodialysis. www.kidney.org/atoz/content/dietary_hemodialysis. Updated April 2019. Accessed September 8, 2023. | ||
| ||
Review Date: 8/28/2023 Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Low sodium diet
Low sodium diet Fruits and vegetab...
Fruits and vegetab...
