Pregnancy SmartSiteTM
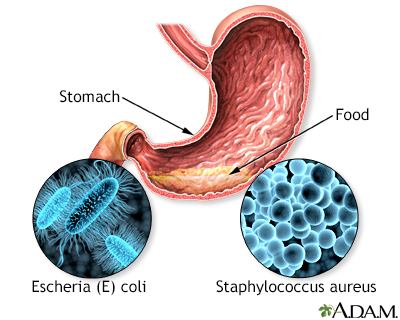
DefinitionFood poisoning occurs when you swallow food or water that contains bacteria, parasites, viruses, or the toxins made by these germs. Most cases are caused by common bacteria such as staphylococcus or E coli. CausesFood poisoning can affect one person or a group of people who all ate the same food. It is more common after eating at picnics, school cafeterias, large social functions, or restaurants. When germs get into the food, it is called contamination. This can happen in different ways:
Food poisoning can occur after eating or drinking:
Many types of germs and toxins may cause food poisoning, including:
Infants and older people are at the greatest risk for food poisoning. You are also at higher risk if:
Pregnant and breastfeeding women should use extra care to avoid food poisoning. SymptomsSymptoms from the most common types of food poisoning will often start within 2 to 6 hours of eating the food. That time may be longer or shorter, depending on the cause of the food poisoning. Possible symptoms include:
Exams and TestsYour health care provider will look for signs of food poisoning. These may include pain in the stomach and signs your body has too little fluid (dehydration). Tests may be done on your stools or the food you have eaten to find out what type of germ is causing your symptoms. However, tests may not always find the cause of the diarrhea. In more serious cases, your provider may order a sigmoidoscopy. This test uses a thin, hollow tube with a light on the end that is placed in the anus and slowly advanced to the rectum and sigmoid colon to look for the source of bleeding or infection. TreatmentMost of the time, you will get better in a couple of days. The goal is to ease symptoms and make sure your body has the proper amount of fluids. Getting enough fluids and learning what to eat will help keep you comfortable. You may need to:
You can drink oral rehydration mixtures to replace fluids and minerals lost through vomiting and diarrhea. Oral rehydration powder can be purchased from a pharmacy. Be sure to mix the powder in safe water. You can make your own mixture by dissolving ½ teaspoon (tsp) or 3 grams (g) salt and ½ tsp (2.3 grams) baking soda and 4 tablespoon (tbsp) or 50 grams of sugar in 4¼ cups (1 liter) water. If you have diarrhea and are unable to drink or keep down fluids, you may need fluids given through a vein (by IV). This may be more common in young children. If you take diuretics ("water pills"), or ACE inhibitors for high blood pressure, contact your provider to see if you need to stop taking the medicine while you have diarrhea. Never stop or change medicines before talking to your provider. For the most common causes of food poisoning, your provider will NOT prescribe antibiotics. You can buy medicines at the drugstore that help slow diarrhea.
Outlook (Prognosis)Most people fully recover from the most common types of food poisoning within 12 to 48 hours. Some types of food poisoning can cause serious complications. Death from food poisoning in people who are otherwise healthy is rare in the United States. Possible ComplicationsDehydration is the most common complication. This can occur from any causes of food poisoning. Less common, but much more serious complications depend on the bacteria that are causing the food poisoning. These may include:
When to Contact a Medical ProfessionalContact your provider if you have:
PreventionThere are many steps that may be taken to prevent food poisoning. ReferencesBrook I. Other clostridium species. In: Long SS, ed. Principles and Practice of Pediatric Infectious Diseases. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 191. Kotloff KL. Acute gastroenteritis in children. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 366. Nguyen T, Akhtar S. Gastroenteritis. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 80. Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 16. Wong KK, Griffin PM. Foodborne disease. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 101. | ||
| ||
Review Date: 12/31/2023 Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Food poisoning
Food poisoning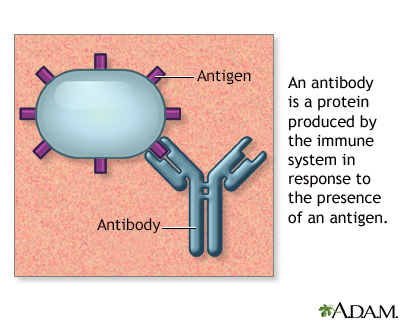 Antibodies
Antibodies
