Pregnancy SmartSiteTM
MPS III; Sanfilippo syndrome; MPS IIIA; MPS IIIB; MPS IIIC; MPS IIID; Lysosomal storage disease - mucopolysaccharidosis type III DefinitionMucopolysaccharidosis type III (MPS III) is a rare disease in which the body is missing or does not have enough of certain enzymes needed to break down long chains of sugar molecules. These chains of molecules are called glycosaminoglycans (formerly called mucopolysaccharides). As a result, the molecules build up in different parts of the body and cause various health problems. The condition belongs to a group of diseases called mucopolysaccharidoses (MPSs). MPS III is also known as Sanfilippo syndrome. There are several other types of MPSs, including:
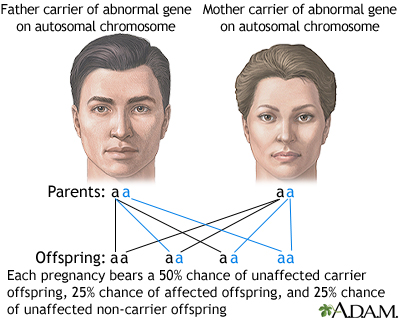
CausesMPS III is an inherited disorder. This means it is typically passed down through families. If both parents carry a nonworking copy of a gene related to this condition, each of their children has a 25% (1 in 4) chance of developing the disease. This is called an autosomal recessive trait. MPS III occurs when the enzymes needed to break down the heparan sulfate sugar chain are missing or defective. There are four main types of MPS III. The type a person has depends on which enzyme is affected.
SymptomsSymptoms often appear after the first year of life. A decline in learning ability typically occurs between ages 2 and 6. The child may have normal growth during the first few years, but final height is below average. Delayed development is followed by worsening mental status. Other symptoms may include:
Exams and TestsYour health care provider will perform a physical exam. Urine tests will be done. People with MPS III have a large amount of a mucopolysaccharide called heparan sulfate in the urine. Other tests may include:
TreatmentTreatment of MPS III is aimed at managing the symptoms. There is no specific treatment for this disease. New research is under development for gene therapy and enzyme replacement. Support GroupsMore information and support for people with MPS III and their families can be found at:
Outlook (Prognosis)MPS III causes significant nervous system symptoms, including severe intellectual disability. Most people with MPS III live into their teenage years. Some live longer, while others with severe forms die at an earlier age. Symptoms are most severe in people with type A. Possible ComplicationsThese complications can occur:
When to Contact a Medical ProfessionalContact your child's provider if your child does not seem to be growing or developing normally. See your provider if you plan to have children and you have a family history of MPS III. PreventionGenetic counseling is recommended for couples who want to have children and who have a family history of MPS III. Prenatal testing is available. ReferencesKumar V, Abbas AK, Aster JC. Genetic disorders. In: Kumar V, Abbas AK, Aster JC, eds. Robbins & Cotran Pathologic Basis of Disease. 10th ed. Philadelphia, PA: Elsevier; 2021:chap 5. Lampe C. Mucopolysaccharidoses. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 109. Pyeritz RE. Inherited diseases of connective tissue. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 239. Turnpenny PD, Ellard S, Cleaver R. Inborn errors of metabolism. In: Turnpenny PD, Ellard S, Cleaver R, eds. Emery's Elements of Medical Genetics and Genomics. 16th ed. Philadelphia, PA: Elsevier; 2022:chap 18. | ||
| ||
Review Date: 4/8/2025 Reviewed By: Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Autosomal recessiv
Autosomal recessiv
