Pregnancy SmartSiteTM
Hyperparathyroidism - parathyroid adenoma; Overactive parathyroid gland - parathyroid adenoma; Osteoporosis - parathyroid adenoma; Bone thinning - parathyroid adenoma; Osteopenia - parathyroid adenoma; High calcium level - parathyroid adenoma; Chronic kidney disease - parathyroid adenoma; Kidney failure - parathyroid adenoma DefinitionA parathyroid adenoma is a noncancerous (benign) tumor of the parathyroid glands. The parathyroid glands are located in the neck, near or attached to the back side of the thyroid gland. CausesThe parathyroid glands in the neck help regulate calcium absorption, use, and removal by the body. They do this by producing parathyroid hormone, or PTH. PTH helps regulate calcium, phosphorus, and vitamin D levels in the blood and bone. It is important for healthy bones. Parathyroid adenomas are common. Most parathyroid adenomas do not have an identified cause. Sometimes a genetic problem is the cause. This is more common if the diagnosis is made when you are young. Parathyroid adenomas may occur in people without a family history of the disease, or as part of 3 inherited syndromes:
In people with an inherited syndrome, a changed (variant) gene is passed down through the family. You only need to get the gene from one parent to develop the condition.
Conditions that stimulate the parathyroid glands to get bigger can also cause an adenoma. These include:
Women over age 60 have the highest risk for developing this condition. Radiation to the head or neck also increases the risk. SymptomsMany people have no symptoms. The condition is often discovered when blood tests are done for another medical reason. Parathyroid adenomas are the most common cause of hyperparathyroidism (overactive parathyroid glands), which leads to an increased blood calcium level. Symptoms may include any of the following:
Exams and TestsBlood tests may be done to check levels of:
Other tests include:
TreatmentSurgery is the most common treatment, and it often cures the condition. But, some people choose to only have regular checkups with their health care provider if the condition is mild. To help improve the condition, your provider may ask you to stop taking calcium and vitamin D supplements. Women who have gone through menopause may want to discuss treatment with estrogen or other medicines to prevent bone loss. Outlook (Prognosis)When treated, outlook is generally good. Possible ComplicationsOsteoporosis and the increased risk for bone fractures is the most common concern. Other complications are less common, but may include:
Complications from surgery include:
When to Contact a Medical ProfessionalContact your provider if you have symptoms of this condition. ReferencesReid LM, Kamani D, Randolph GW. Management of parathyroid disorders. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 123. Thakker RV. The parathyroid glands, hypercalcemia, and hypocalcemia. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 227. Walker MD, Bilezikian JP. Primary hyperparathyroidism. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 54. | ||
| ||
Review Date: 5/20/2024 Reviewed By: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


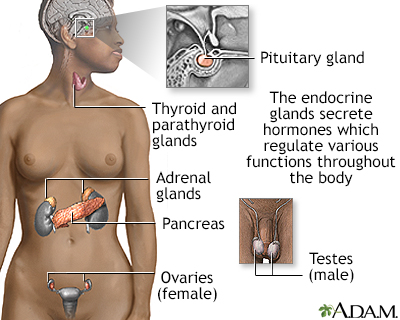 Endocrine glands
Endocrine glands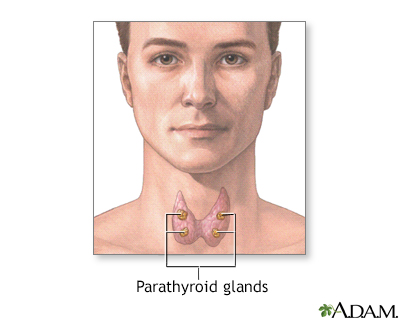 Parathyroid glands
Parathyroid glands
