Pregnancy SmartSiteTM
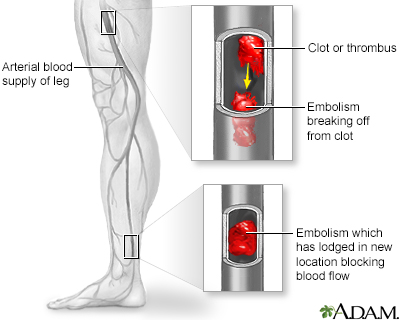
DefinitionArterial embolism refers to a clot (embolus) that has come from another part of the body and causes a sudden interruption of blood flow to an organ or body part. CausesAn "embolus" is a blood clot or a piece of atherosclerotic plaque that acts like a clot. The word "emboli" means there is more than one clot or piece of plaque. When the clot travels from the site where it formed to another location in the body, it is called an embolism. An arterial embolism may be caused by one or more clots. The clots can get stuck in an artery and block blood flow. The blockage starves tissues of blood and oxygen. This can result in damage or tissue death (necrosis). Arterial emboli often occur in the legs and feet. Emboli that occur in the brain cause a stroke. Ones that occur in the heart cause a heart attack. Other sites include the kidneys, intestines, and eyes. Risk factors for arterial embolism include:
Another condition that poses a high risk for embolization (especially to the brain) is mitral stenosis. Endocarditis (infection of the inside of the heart) can also cause arterial emboli. A common source for an embolus is from areas of hardening (atherosclerosis causing plaque) in the aorta and other large blood vessels. These clots can break loose and flow down to the abdominal organs, legs and feet. Paradoxical embolization can take place when a clot in a vein enters the right side of the heart and passes through a hole into the left side of the heart. The clot can then move to an artery and block blood flow to the brain (stroke) or other organs. If a clot travels and lodges in the arteries supplying blood flow to the lungs, it is called a pulmonary embolus. SymptomsYou may not have any symptoms. Symptoms may begin quickly or slowly depending on the size of the embolus and how much it blocks the blood flow. Symptoms of an arterial embolism in the arms or legs may include:
Later symptoms:
Symptoms of a clot in an organ vary with the organ involved but may include:
Exams and TestsThe health care provider may find decreased or no pulse, and decreased or no blood pressure in the arm or leg. There may be signs of tissue death or gangrene. Tests to diagnose arterial embolism or reveal the source of emboli may include:
This disease may also affect the results of the following tests:
TreatmentArterial embolism requires prompt treatment at a hospital. The goals of treatment are to control symptoms and to improve the interrupted blood flow to the affected area of the body. The cause of the clot, if found, should be treated to prevent further problems. Medicines include:
Some people need surgery. Procedures include:
Outlook (Prognosis)How well a person does depends on the location of the clot and how much the clot has blocked blood flow and for how long the blockage has been present. Arterial embolism can be very serious if not treated promptly. The affected area can be permanently damaged. Amputation is needed in up to 1 in 4 cases. Arterial emboli can come back even after successful treatment. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalGo to the emergency room or call 911 or the local emergency number if you have symptoms of arterial embolism. PreventionPrevention begins with finding possible sources of a blood clot. Your provider may prescribe blood thinners (such as warfarin or heparin) to prevent clots from forming. Antiplatelet drugs may also be needed. You have a higher risk atherosclerosis and clots if you:
ReferencesAufderheide TP. Peripheral arteriovascular disease. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 73. Goldman L. Approach to the patient with possible cardiovascular disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 39. Gornik, H, Aronow, H. et al. 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS Guideline for the Management of Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. Available online 14 May 2024. doi.org/10.1016/j.jacc.2024.02.013. pubmed.ncbi.nlm.nih.gov/38743805/. Kabrhel C. Pulmonary embolism and deep vein thrombosis. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 74. Zettervall SL, Schemerhorm ML. Acute mesenteric arterial disease: epidemiology, pathophysiology, clinical evaluation, and management. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 133. | ||
| ||
Review Date: 5/8/2024 Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Arterial embolism
Arterial embolism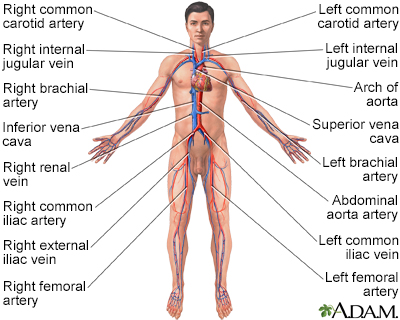 Circulatory system
Circulatory system
