Pregnancy SmartSiteTM
Conjunctivitis - allergic seasonal/perennial; Atopic keratoconjunctivitis; Pink eye - allergic DefinitionThe conjunctiva is a clear layer of tissue lining the eyelids and covering the white of the eye. Allergic conjunctivitis occurs when the conjunctiva becomes swollen or inflamed due to a reaction to pollen, dust mites, pet dander, mold, or other allergy-causing substances. CausesWhen your eyes are exposed to allergens (which cause allergies), a substance called histamine is released by your body. The blood vessels in the conjunctiva become swollen. The eyes can become red, itchy, and teary very quickly. The pollens that cause symptoms vary from person to person and from area to area. Tiny pollens that may cause allergic symptoms include grasses, ragweed and trees. These same pollens may also cause hay fever. Your symptoms may be worse when there is more pollen in the air. Higher levels of pollen are more likely on hot, dry, windy days. On cool, damp, rainy days most pollen is washed to the ground. Mold, animal dander, or dust mites may cause this problem also. Allergies tend to run in families. It is hard to know exactly how many people have allergies. Many conditions are often lumped under the term "allergy" even when they might not truly be an allergy. SymptomsSymptoms may be seasonal and can include:
Exams and TestsYour health care provider may look for the following:
Allergy testing may identify the pollen or other substances that trigger your symptoms.
TreatmentThe best treatment is to avoid what causes your allergy symptoms as much as possible. Common triggers to avoid include dust, mold and pollen. Some things you can do to ease symptoms are:
If home-care does not help, you may need to see a provider for treatments such as eye drops that contain antihistamines or eye drops that reduce swelling. Mild steroid eye drops can be prescribed for more severe reactions. You may also use eye drops that prevent a type of white blood cell called mast cells from causing swelling. These drops are given along with antihistamines. These medicines work best if you take them before you come in contact with the allergen. Referral to an ophthalmologist before using steroid eye drops should be done since intraocular pressure measurements and a more thorough eye exam (using a slit lamp) is needed. Outlook (Prognosis)Symptoms often go away with treatment. However, they can persist if you continue to be exposed to the allergen. Long-term swelling of the outer lining of the eyes may occur in those with chronic allergies or asthma. It is called vernal conjunctivitis. It is most common in young males, and most often occurs during the spring and summer. Possible ComplicationsIn severe cases of allergic conjunctivitis, there could be more severe inflammation. This can, rarely, affect your vision. When to Contact a Medical ProfessionalContact your provider if:
ReferencesCioffi GA, Liebmann JM. Diseases of the visual system. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 391. Rubenstein JB, Patel P. Allergic conjunctivitis. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 4.7. | ||
| ||
Review Date: 7/22/2024 Reviewed By: Deborah Pedersen, MD, MS, Allergy & Asthma Care, PC, Taunton, MA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


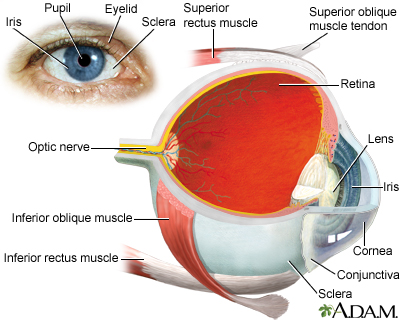 Eye
Eye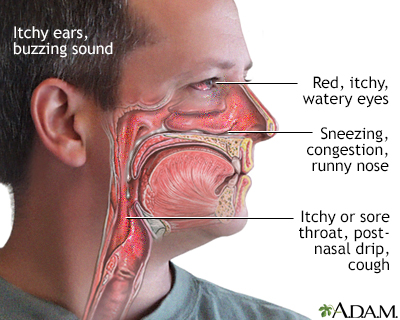 Allergy symptoms
Allergy symptoms Conjunctivitis
Conjunctivitis
