Pregnancy SmartSiteTM
Developmental dislocation of the hip joint; Developmental hip dysplasia; DDH; Congenital dysplasia of the hip; Congenital dislocation of the hip; CDH; Pavlik harness DefinitionDevelopmental dysplasia of the hip (DDH) is a dislocation of the hip joint that is present at birth. The condition is found in babies or young children. CausesThe hip is a ball and socket joint. The ball is called the femoral head. It forms the top part of the thigh bone (femur). The socket (acetabulum) forms in the pelvic bone. In some newborns, the socket is too shallow and the ball (thigh bone) may slip out of the socket, either part of the way or completely. One or both hips may be involved. The cause is unknown. Low levels of amniotic fluid in the womb during pregnancy can increase a baby's risk for DDH. Other risk factors include:
DDH occurs in about 1 to 1.5 of 1,000 births. SymptomsThere may be no symptoms. Symptoms that may occur in a newborn can include:
After 3 months of age, the affected leg may turn outward or be shorter than the other leg. Once the child begins walking, symptoms can include:
Exams and TestsPediatric health care providers routinely screen all newborns and infants for hip dysplasia. There are several methods to detect a dislocated hip or a hip that is able to be dislocated. The most common method of identifying the condition is a physical exam of the hips, which involves applying pressure while moving the hips. The provider listens for any clicks, clunks, or pops. Ultrasound of the hip is used in younger infants to confirm the problem. An x-ray of the hip joint may help diagnose the condition in older infants and children. A hip that is truly dislocated in an infant should be detected at birth, but some cases are mild and symptoms may not develop until after birth, which is why multiple exams are recommended. Some mild cases are silent and cannot be found during a physical exam. TreatmentWhen the problem is found during the first 6 months of life, a device or harness is used to keep the legs apart and turned outward (frog-leg position). This device will most often hold the hip joint in place while the child grows. This harness works for most infants when it is started before age 6 months, but it is less likely to work for older children. Children who do not improve or who are diagnosed after 6 months often need surgery. After surgery, a cast will be placed on the child's leg for a period of time. Outlook (Prognosis)If hip dysplasia is found in the first few months of life, it can almost always be treated successfully with a positioning device (bracing). In a few cases, surgery is needed to put the hip back in joint. Hip dysplasia that is found after early infancy may lead to a worse outcome and may need more complex surgery to fix the problem. Possible ComplicationsBracing devices may cause skin irritation. Differences in the lengths of the legs may persist despite appropriate treatment. Untreated, hip dysplasia will lead to arthritis and deterioration of the hip, which can be severely debilitating. When to Contact a Medical ProfessionalContact your provider if you suspect that your child's hip is not properly positioned. ReferencesKelly DM. Congenital and developmental abnormalities of the hip and pelvis. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 30. Sankar WN, Winell JJ, Horn BD, Wells L. The hip. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 719. Son-Hing JP, Hardesty CK. Congenital abnormalities of the upper and lower extremities and spine. In: Martin RJ, Fanaroff AA, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 103. | ||
| ||
Review Date: 1/1/2025 Reviewed By: Charles I. Schwartz, MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


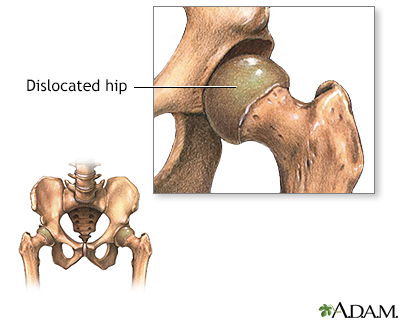 Congenital hip dis...
Congenital hip dis...
