Pregnancy SmartSiteTM
Pelvic pain - endometriosis; Endometrioma DefinitionEndometriosis occurs when cells from the lining of your womb (uterus) grow in other areas of your body. This can cause pain, heavy vaginal bleeding, vaginal bleeding between periods, and problems getting pregnant (infertility). CausesEvery month, a woman's ovaries produce hormones that tell the cells lining the uterus to swell and get thicker. Your uterus sheds these cells along with blood and tissue through your vagina when you have your period. Endometriosis occurs when these cells grow outside the uterus in other parts of your body. This tissue may attach on your:
It can grow in other areas of the body, too. These growths stay in your body, and like the cells in the lining of your uterus, these growths react to the hormones from your ovaries. This may cause you to have pain during the month prior to the onset of your period. Over time, the growths may add more tissue and blood. Growths can also build up in the abdomen and pelvis, leading to chronic pelvic pain, heavy menstrual cycles, and infertility. The cause of endometriosis is unknown. One idea is that when you get your period, the cells may travel backwards through the fallopian tubes into the pelvis. Once there, the cells attach and grow. However, this backward period flow occurs in many women. The immune system may play a role in causing endometriosis in women with the condition. Endometriosis is common. It occurs in about 10% of women of reproductive age. Sometimes, it may run in families. Endometriosis probably starts when a woman begins having periods. However, it usually is not diagnosed until ages 25 to 40. You are more likely to develop endometriosis if you:
SymptomsPain is the main symptom of endometriosis. You may have:
Other symptoms of endometriosis include:
You may not have any symptoms. Some women with a lot of tissue in their pelvis have no pain at all, while some women with milder disease have severe pain. Exams and TestsYour health care provider will perform a physical exam, including a pelvic exam. You may have one of these tests to help diagnose the disease:
TreatmentLearning how to manage your symptoms can make it easier to live with endometriosis. What type of treatment you have depends on:
There is currently no cure for endometriosis. There are different treatment options. PAIN RELIEVERS If you have mild symptoms, you may be able to manage cramping and pain with:
HORMONE THERAPY These medicines can stop endometriosis from getting worse. They may be given as pills, nasal spray, or shots. Only women who are not trying get pregnant should have this therapy. Some types of hormone therapy will also prevent you from getting pregnant while you are taking the medicine. Birth control pills -- With this therapy, you take the hormone pills (not the inactive or placebo pills) for 6 to 9 months continuously. Taking these pills relieves most symptoms. However, it does not treat any damage that has already occurred. But it may prevent ongoing damage for as long as the hormone-containing pills are taken. Many young patients will choose to continue this treatment indefinitely or until they wish to attempt pregnancy. Progesterone pills, injections, or intrauterine device (IUD) -- This treatment helps shrink endometrial growths. Side effects may include weight gain and depression. Gonadotropin-agonist medicines -- These medicines stop your ovaries from producing the hormone estrogen. This causes a menopause-like state. Side effects include hot flashes, vaginal dryness, and mood changes. Treatment is often limited to 6 months because it can weaken your bones. Your provider may give you small doses of an estrogen hormone to relieve symptoms during this treatment. This is known as 'add-back' therapy. It may also help protect against bone loss, while not triggering growth of the endometriosis. Gonadotropin-antagonist medicine -- This oral medication helps lower production of estrogen resulting in a menopausal-like state and controls the growth of endometrial tissue, resulting in less severe painful and heavy menstrual periods. SURGERY Your provider may recommend surgery if you have severe pain that does not get better with other treatments.
Laparoscopy or laparotomy may be a good option if you want to become pregnant, because they treat the disease and leave your organs in place. Outlook (Prognosis)There is no cure for endometriosis. Hormone therapy can help relieve symptoms, but symptoms often return when therapy is stopped. Surgical treatment may help relieve symptoms for years. However, not all women with endometriosis are helped by these treatments. Once you enter menopause, endometriosis is unlikely to cause problems. Possible ComplicationsEndometriosis can lead to problems getting pregnant. However, most women with mild symptoms can still get pregnant. Laparoscopy to remove growths and scar tissue may help improve your chances of becoming pregnant. If it does not, you may want to consider fertility treatments. Other complications of endometriosis include:
In rare cases, endometriosis tissue may block the intestines or urinary tract. Very rarely, cancer may develop in the areas of tissue growth after menopause. When to Contact a Medical ProfessionalContact your provider if:
You may want to get checked for endometriosis if:
PreventionBirth control pills may help to prevent or slow down the development of the endometriosis. Birth control pills used as treatment for endometriosis work best when taken continuously and not stopped to allow a menstrual period. They may be used for young women in late adolescence or early 20s with painful periods that may be due to endometriosis. ReferencesAdvincula A, Truong M, Lobo RA. Endometriosis: etiology, pathology, diagnosis, management. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 19. Burney RO, Giudice LC. Endometriosis. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 125. Kalaitzopoulos DR, Samartzis N, Kolovos GN, et al. Treatment of endometriosis: a review with comparison of 8 guidelines. BMC Womens Health. 2021;21(1):397. PMID: 34844587 pubmed.ncbi.nlm.nih.gov/34844587/. Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382(13):1244-1256. PMID: 32212520 pubmed.ncbi.nlm.nih.gov/32212520/. | ||
| ||
Review Date: 5/22/2025 Reviewed By: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


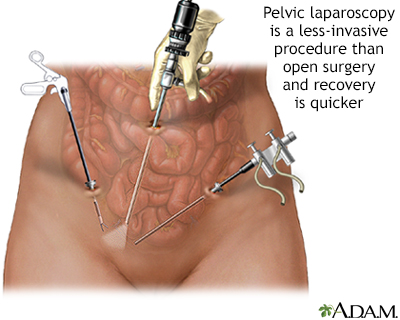 Pelvic laparoscopy
Pelvic laparoscopy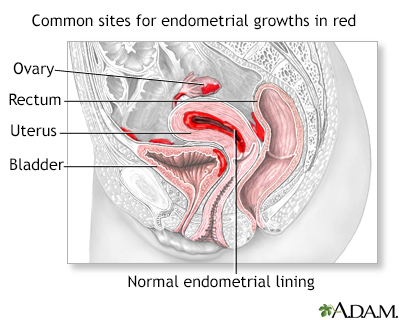 Endometriosis
Endometriosis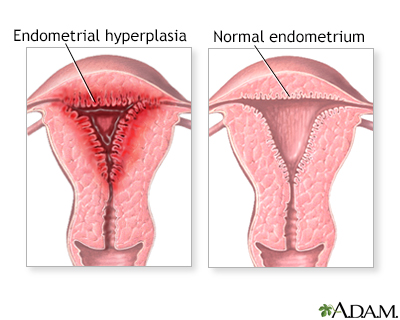 Abnormal menstrual...
Abnormal menstrual...
