Pregnancy SmartSiteTM
PID; Oophoritis; Salpingitis; Salpingo - oophoritis; Salpingo - peritonitis DefinitionPelvic inflammatory disease (PID) is an infection of a woman's womb (uterus), ovaries, or fallopian tubes. CausesPID is an infection caused by bacteria. When bacteria from the vagina or cervix travel to your womb, fallopian tubes, or ovaries, they can cause an infection. Most of the time, PID is caused by the bacteria chlamydia or gonorrhea. These are sexually transmitted infections (STIs). Having unprotected sex with someone who has an STI can cause PID. Bacteria normally found in the cervix can also travel into the uterus and fallopian tubes during a medical procedure such as:
In the United States, nearly 1 million women have PID each year. About 1 in 8 sexually active women will have PID before age 20. You are more likely to get PID if:
SymptomsCommon symptoms of PID include:
Other symptoms that may occur with PID:
You can have PID and not have any severe symptoms. For example, chlamydia can cause PID with no symptoms. Women who have an ectopic pregnancy or who are infertile often have PID caused by chlamydia. An ectopic pregnancy is when an egg grows outside of the uterus. It puts the mother's life in danger. Exams and TestsYour health care provider may do a pelvic exam to look for:
You may have lab tests to check for signs of body-wide infection: Other tests include:
TreatmentYour provider will often have you start taking antibiotics while waiting for your test results. If you have mild PID:
If you have more severe PID:
There are many different antibiotics that can treat PID. Some are safe for pregnant women. Which type you take depends on the cause of the infection. You may receive a different treatment if you have gonorrhea or chlamydia. Finishing the full course of antibiotics you've been given is extremely important for treating PID. Scarring inside the womb or of the tubes from PID may lead to the need to have surgery or undergo invitro fertilization (IVF) to become pregnant. Follow up with your provider after you've finished the antibiotics to make sure that you no longer have the bacteria in your body. It's very important that you practice safe sex in order to reduce your risk of getting infections, which could lead to PID. If your PID is caused by an STI like gonorrhea or chlamydia, your sexual partner must be treated as well.
Possible ComplicationsPID infections can cause scarring of the pelvic organs. This can lead to:
If you have a serious infection that does not improve with antibiotics, you may need surgery. When to Contact a Medical ProfessionalContact your provider if:
PreventionGet prompt treatment for STIs. You can help prevent PID by practicing safer sex.
Here is how you can reduce your risk for PID:
ReferencesCenters for Disease Control and Prevention website. Sexually transmitted infections treatment guidelines, 2021. www.cdc.gov/std/treatment-guidelines/default.htm. Updated June 13, 2023. Accessed September 27, 2023. Lipsky AM, Hart D. Acute pelvic pain. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 29. McKinzie J. Sexually transmitted infections. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 84. Prescott LS, Yunker AC, Alvarez R. Gynecologic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 71. | ||
| ||
Review Date: 7/12/2023 Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


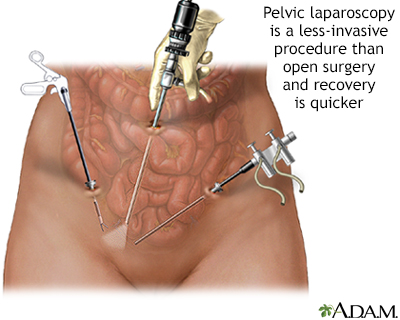 Pelvic laparoscopy
Pelvic laparoscopy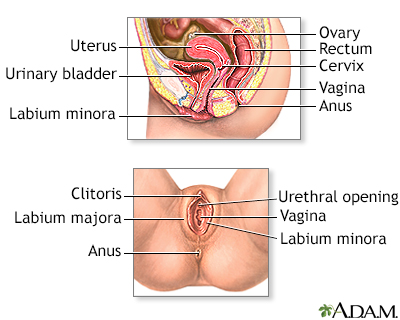 Female reproductiv...
Female reproductiv...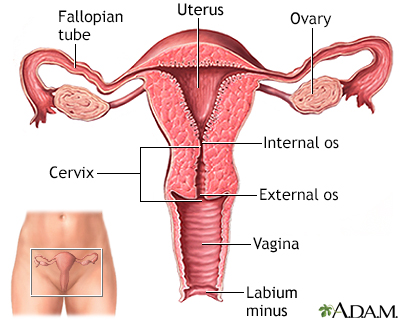 Uterus
Uterus
