Pregnancy SmartSiteTM
Primary syphilis; Secondary syphilis; Late syphilis; Tertiary syphilis; Treponema - syphilis; Lues; Sexually transmitted disease - syphilis; Sexually transmitted infection - syphilis; STD - syphilis; STI - syphilis DefinitionSyphilis is a bacterial infection that is most often spread through sexual contact. CausesSyphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. This bacterium causes infection when it gets into broken skin or mucus membranes, usually of the genitals. Syphilis is most often transmitted through sexual contact, although it also can be transmitted in other ways. Syphilis occurs worldwide, most commonly in urban areas. The number of cases is rising fastest in men who have sex with men (MSM). Young adults ages 20 to 35 are the highest-risk population. Because people may be unaware that they are infected with syphilis, many states require tests for syphilis before marriage. All pregnant women who receive prenatal care should be screened for syphilis to prevent the infection from passing to their newborn (congenital syphilis). Also, people at increased risk for getting syphilis should be screened for it. Syphilis has three stages:
Secondary syphilis, tertiary syphilis, and congenital syphilis are not seen as often in the United States because of education, screening, and treatment. SymptomsThe incubation period for primary syphilis is 14 to 21 days. Symptoms of primary syphilis are:
The bacteria continue to grow in the body, but there are few symptoms until the second stage. The symptoms of secondary syphilis start 4 to 8 weeks after the primary syphilis. The symptoms may include:
Primary and secondary syphilis usually resolve without treatment. At that point, syphilis becomes latent and may have no symptoms for many years. But, during this time, it may be damaging organs leading to tertiary syphilis. Tertiary syphilis develops in untreated people. The symptoms depend on which organs have been affected. They vary widely and can be difficult to diagnose. Symptoms include:
Exams and TestsYour health care provider will perform a physical exam and ask about the symptoms. Tests that may be done include:
If the RPR, VDRL, or TRUST tests are positive, additional tests will be done to confirm the diagnosis: TreatmentSyphilis can be treated with antibiotics, such as:
The length of treatment depends on how severe the syphilis is, and factors such as the person's overall health. To treat syphilis during pregnancy, penicillin is the medicine of choice. Tetracycline cannot be used for treatment because it is dangerous to the unborn baby. Erythromycin may not prevent congenital syphilis in the baby. People who are allergic to penicillin should ideally be desensitized to it, and then treated with penicillin. Several hours after getting treatment for the early stages of syphilis, people may experience the Jarisch-Herxheimer reaction. This process is caused by an immune reaction to the breakdown products of the infection and not an allergic reaction to the antibiotic. Symptoms and signs of this reaction include:
These symptoms usually disappear within 24 hours. Follow-up blood tests must be done at 3, 6, 12, and 24 months to ensure that the infection is gone. Avoid sexual contact when the chancre is present. Use condoms until two follow-up tests have shown that the infection has been cured, to reduce the chance of transmitting the infection. All sexual partners of the person with syphilis should also be treated. Syphilis can spread very easily in the primary and secondary stages. Outlook (Prognosis)Primary and secondary syphilis can be cured if it is diagnosed early and completely treated. Although secondary syphilis usually goes away within weeks, in some cases it may last for up to 1 year. Without treatment, up to one-third of people will have late complications of syphilis. Tertiary syphilis may be permanently disabling, and it may lead to death. Possible ComplicationsComplications of syphilis may include:
In addition, untreated secondary syphilis during pregnancy may spread the disease to the developing baby. This is called congenital syphilis. When to Contact a Medical ProfessionalContact your provider for an appointment if you have symptoms of syphilis. Also contact your provider or get screened at an STI clinic if you have:
PreventionIf you are sexually active, practice safer sex and always use a condom. All pregnant women should be screened for syphilis. Also, people at increased risk for getting syphilis should be screened for it. Common examples include men who have sex with men, people with HIV infection, young adults, and people with a history of incarceration, sex work, military service or illicit drug use. ReferencesDionne JA, Ghanem KG. Syphilis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 295. Radolf JD, Tramont EC, Salazar JC. Syphilis (Treponema pallidum). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 237. Stary G, Stary A. Sexually transmitted infections. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier; 2025:chap 82. US Preventive Services Task Force website. Syphilis infection in nonpregnant adolescents and adults: Screening. www.uspreventiveservicestaskforce.org/uspstf/announcements/final-recommendation-statement-screening-syphilis-infection-nonpregnant-adolescents-and-adults. Updated September 27, 2022. Accessed November 9, 2024. | ||
| ||
Review Date: 8/29/2024 Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


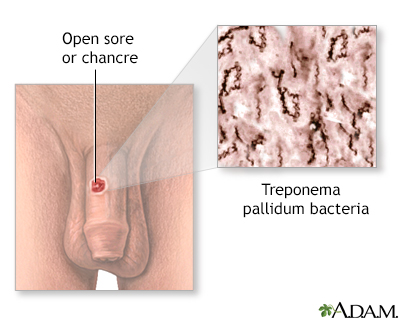 Primary syphilis
Primary syphilis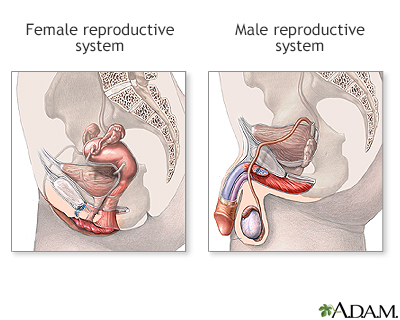 Male and female re...
Male and female re... Syphilis - seconda...
Syphilis - seconda...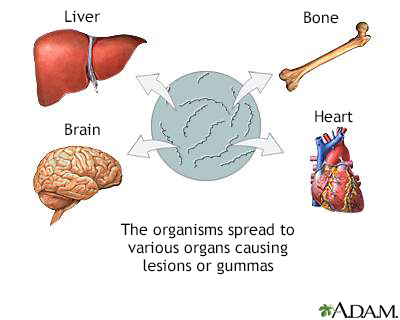 Late-stage syphili
Late-stage syphili
