Pregnancy SmartSiteTM
Shy-Drager syndrome; Neurologic orthostatic hypotension; Shy-McGee-Drager syndrome; Parkinson plus syndrome; MSA-P; MSA-C DefinitionMultiple system atrophy- parkinsonian type (MSA-P) is a rare condition that causes symptoms similar to Parkinson disease. However, people with MSA-P have more widespread damage to the part of the nervous system that regulates important functions such as heart rate, blood pressure, and sweating. The other subtype of MSA is MSA-cerebellar. It mainly affects the cerebellum, an area deep in the brain, just above the spinal cord. CausesThe cause of MSA-P is unknown. The affected areas of the brain overlap with areas affected by Parkinson disease, with similar symptoms. For this reason, this subtype of MSA is called parkinsonian. MSA-P is most often diagnosed in men older than 60. SymptomsMSA damages the nervous system. The disease tends to progress rapidly. About one half of people with MSA-P have lost most of their motor skills within 5 years of onset of the disease. Symptoms may include:
Other symptoms that may occur with this disease:
Exams and TestsYour health care provider will examine you, and check your eyes, nerves, and muscles. Your blood pressure will be taken while you are lying down and standing up. There are no specific tests to confirm this disease. A specialist in the nervous system (neurologist) can make the diagnosis based on:
Testing to help confirm the diagnosis may include:
TreatmentThere is no cure for MSA-P. There is no known way to prevent the disease from getting worse. The goal of treatment is to control symptoms. Dopaminergic medicines, such as levodopa and carbidopa, may be used to reduce early or mild tremors. But, for many people with MSA-P, these medicines do not work well. Medicines may be used to treat low blood pressure. A pacemaker that is programmed to stimulate the heart to beat at a rapid rate (faster than 100 beats per minute) may increase blood pressure for some people. Constipation can be treated with a high-fiber diet and laxatives. Medicines are available to treat erection problems. Support GroupsMore information and support for people with MSA-P and their families can be found at:
Outlook (Prognosis)The outcome for MSA is poor. Loss of mental and physical functions slowly get worse. Early death is likely. People typically live 7 to 9 years after diagnosis. When to Contact a Medical ProfessionalContact your provider if you develop symptoms of this disorder. Contact your provider if you have been diagnosed with MSA and your symptoms return or get worse. Also contact your provider if new symptoms appear, including possible side effects of medicines, such as:
If you have a family member with MSA and their condition declines to the point that you are unable to care for the person at home, seek advice from your family member's provider. ReferencesJankovic J. Parkinson disease and other movement disorders. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 96. National Institutes of Health website. National Institute of Neurological Disorders and Stroke. Multiple system atrophy. www.ninds.nih.gov/health-information/disorders/multiple-system-atrophy. Updated July 19, 2024. Accessed November 4, 2024. Romero-Ortuno R, Wilson KJ, Hampton JL. Disorders of the autonomic nervous system. In: Fillit HM, Rockwood K, Young J, eds. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 8th ed. Philadelphia, PA: Elsevier; 2017:chap 63. | ||
| ||
Review Date: 10/23/2024 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


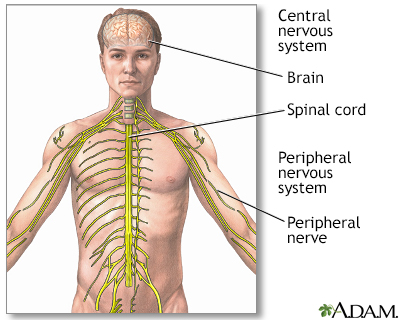 Central nervous sy...
Central nervous sy...
