Pregnancy SmartSiteTM
Cerebrovascular disease; CVA; Cerebral infarction; Cerebral hemorrhage; Ischemic stroke; Stroke - ischemic; Cerebrovascular accident; Stroke - hemorrhagic; Carotid artery - stroke DefinitionA stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack." If blood flow is cut off for longer than a few seconds, the brain cannot get nutrients and oxygen. Brain cells can die, causing lasting damage. A stroke can also occur if a blood vessel inside the brain bursts, leading to bleeding inside the head. CausesThere are two major types of stroke:
Ischemic stroke occurs when a blood vessel that supplies blood to the brain is blocked by a blood clot. This may happen in two ways:
Ischemic strokes may also be caused by a sticky substance called plaque that can clog arteries. A hemorrhagic stroke occurs when a blood vessel in part of the brain becomes weak and bursts open. This causes blood to leak into the brain. Some people have defects in the blood vessels of the brain that make this more likely. These defects may include:
Hemorrhagic strokes may also occur when someone is taking blood thinners, such as dabigatran, rivaroxaban, apixaban, edoxaban and warfarin or has a bleeding disorder. Very high blood pressure may cause blood vessels to burst, leading to hemorrhagic stroke. An ischemic stroke can develop bleeding and become a hemorrhagic stroke. High blood pressure is the main risk factor for strokes. Other major risk factors are:
Stroke risk is also higher in:
SymptomsSymptoms of stroke depend on which part of the brain is damaged. In some cases, a person may not know that a stroke has occurred. Most of the time, symptoms develop suddenly and without warning. But symptoms may occur on and off for the first day or two. Symptoms are usually most severe when the stroke first happens, but they may slowly get worse. A headache may occur if the stroke is caused by bleeding in the brain. The headache:
Other symptoms depend on how severe the stroke is, and what part of the brain is affected. Symptoms may include:
Exams and TestsYour health care provider will do a physical exam to:
You may have the following tests to help find the type, location, and cause of the stroke and check for other problems:
Other tests include:
TreatmentA stroke is a medical emergency. Quick treatment is needed. Call 911 or the local emergency number right away or seek urgent medical care at the first signs of a stroke. People who are having stroke symptoms need to get to a hospital as quickly as possible.
Other treatments given in the hospital depend on the cause of the stroke. These may include:
Physical therapy, occupational therapy, speech therapy, and swallowing therapy will all begin in the hospital. If the person has severe swallowing problems, a feeding tube in the stomach (gastrostomy tube) will likely be needed. The goal of treatment after a stroke is to help you recover as much function as possible and prevent future strokes. Recovery from your stroke will begin while you are still in the hospital or at a rehab center. It will continue when you go home from the hospital or center. Be sure to follow up with your provider after you go home. Support GroupsMore information and support for people with stroke and their families can be found on the American Stroke Association website -- www.stroke.org/en/help-and-support. Outlook (Prognosis)How well a person does after a stroke depends on:
Problems moving, thinking, and talking often start to improve in the days to weeks after a stroke. Many people develop depression after a stroke. This can slow down recovery but is also a very treatable complication of a stroke. Many people who have had a stroke will keep improving in the months or years after their stroke. Over half of people who have a stroke are able to function and live at home. Others are not able to care for themselves. If treatment with clot-busting medicines is successful, the symptoms of a stroke may go away. However, people often do not get to the hospital soon enough to receive these medicines, or they cannot take these medicines because of a health condition. People who have a stroke from a blood clot (ischemic stroke) have a better chance of surviving than those who have a stroke from bleeding in the brain (hemorrhagic stroke). The risk for a second stroke is highest during the weeks or months after the first stroke. The risk begins to decrease after this period. When to Contact a Medical ProfessionalStroke is a medical emergency that needs to be treated right away. The acronym F.A.S.T. is an easy way to remember signs of stroke and what to do if you think a stroke has occurred. The most important action to take is to call 911 or the local emergency number right away for emergency assistance. F.A.S.T. stands for:
PreventionReducing your stroke risk factors lessens your chance of having a stroke. ReferencesBiller J, Schneck MJ, Ruland S. Ischemic cerebrovascular disease. In Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley's and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 65. Bushnell C, Kernan WN, Sharrief AZ, et al. 2024 Guideline for the primary prevention of stroke: a guideline from the American Heart Association/American Stroke Association. Stroke. 2024;55(12):e344-e424. PMID: 39429201 pubmed.ncbi.nlm.nih.gov/39429201/. Chaturvedi S, Selim M. Hemorrhagic cerebrovascular disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 377. Gladstone DJ, Lindsay MP, Douketis J, et al. Canadian stroke consortium. Canadian stroke best practice recommendations: secondary prevention of stroke Update 2020. Can J Neurol Sci. 2022;49(3):315-337. PMID: 34140063 pubmed.ncbi.nlm.nih.gov/34140063/. Goldstein LB. Ischemic cerebrovascular disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 376. Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024;149(1):e1-e156. PMID: 38033089 pubmed.ncbi.nlm.nih.gov/38033089/. Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021;52(7):e-364-e467. PMID: 34024117 pubmed.ncbi.nlm.nih.gov/34024117/. Papa L, Meurer WJ. Stroke. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 87. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. PMID: 31662037 pubmed.ncbi.nlm.nih.gov/31662037/. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;72(3):e127-e248. PMID: 29133354 pubmed.ncbi.nlm.nih.gov/29133354/. | ||
| ||
Review Date: 4/16/2025 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


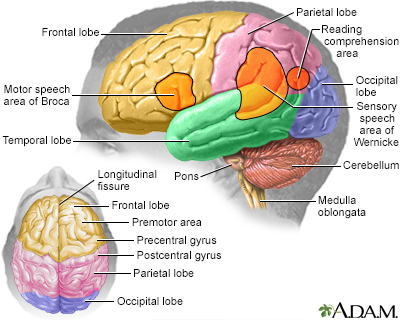 Brain
Brain Carotid stenosis -...
Carotid stenosis -...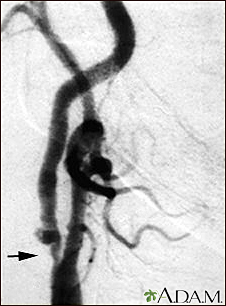 Carotid stenosis -...
Carotid stenosis -...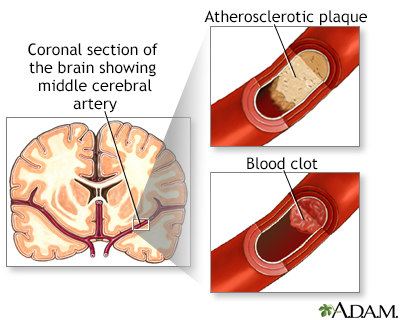 Stroke
Stroke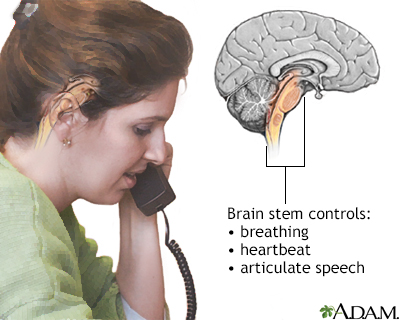 Brainstem function
Brainstem function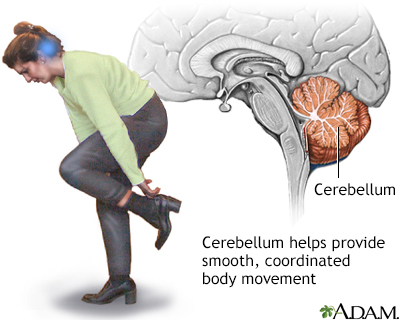 Cerebellum - funct...
Cerebellum - funct...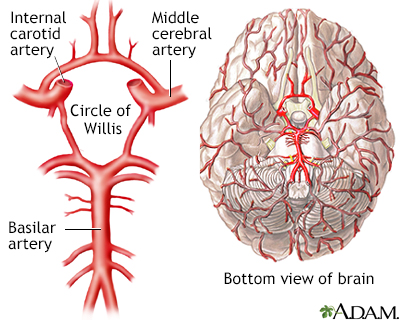 Circle of Willis
Circle of Willis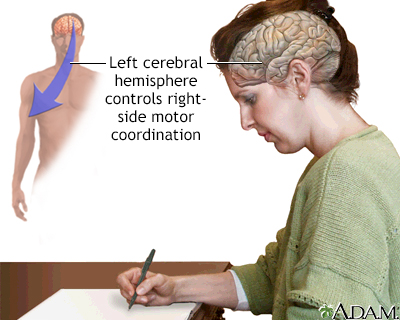 Left cerebral hemi...
Left cerebral hemi...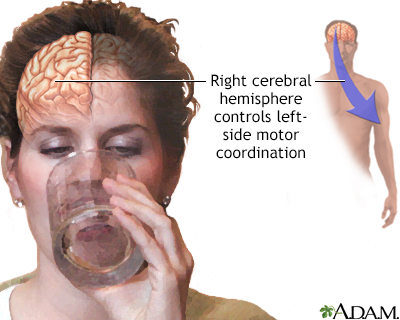 Right cerebral hem...
Right cerebral hem...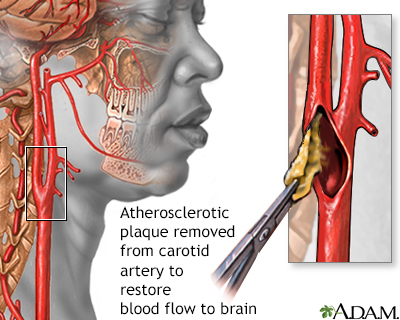 Endarterectomy
Endarterectomy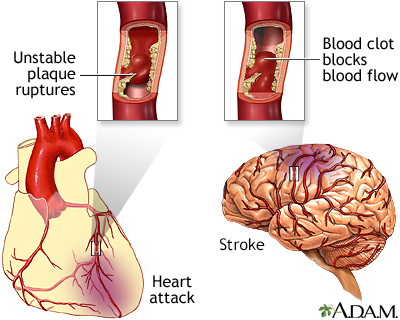 Plaque buildup in ...
Plaque buildup in ...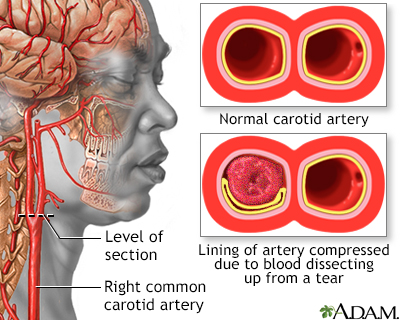 Carotid dissection
Carotid dissection
