Pregnancy SmartSiteTM
Muscular dystrophy - limb-girdle type (LGMD) DefinitionLimb-girdle muscular dystrophies include at least 33 different inherited diseases. These disorders first affect the muscles around the shoulder girdle and hips. These diseases get worse over time. Eventually, it may involve other muscles. CausesLimb-girdle muscular dystrophies are a large group of genetic diseases in which there is muscle weakness and wasting (muscular dystrophy). In most cases, both parents must pass on the non-working (defective) gene for a child to have the disease (autosomal recessive inheritance). In some rare types, only one parent needs to pass on the non-working gene to affect the child. This is called autosomal dominant inheritance. For most of these conditions, the defective gene has been discovered. An important risk factor is having a family member with muscular dystrophy. SymptomsMost often, the first sign is pelvic muscle weakness. Examples of this include trouble standing from a sitting position without using the arms, or difficulty climbing stairs. The weakness starts in childhood to young adulthood. Other symptoms include:
Exams and TestsTests may include:
TreatmentThere are no known treatments that reverse the muscle weakness. Gene therapy may become available in the future. Supportive treatment can decrease the complications of the disease. The condition is managed based on the person's symptoms. It includes:
Surgery is sometimes needed for any bone or joint problems. Support GroupsThe Muscular Dystrophy Association is an excellent resource: www.mda.org Outlook (Prognosis)In general, people tend to have weakness that slowly gets worse in affected muscles and spreads. The disease causes loss of movement. The person may be dependent on a wheelchair within 20 to 30 years. Heart muscle weakness and abnormal electrical activity of the heart can increase the risk for palpitations, fainting, and sudden death. Most people with this group of diseases live into adulthood, but do not reach their full life expectancy. Possible ComplicationsPeople with limb-girdle muscular dystrophies may experience complications such as:
When to Contact a Medical ProfessionalContact your health care provider if you or your child feels weak while rising from a squatting position. Contact a geneticist if you or a family member has been diagnosed with muscular dystrophy, and you are planning a pregnancy. PreventionGenetic counseling is now offered to affected individuals and their families. Soon molecular testing will involve whole genome sequencing on patients and their relatives to better establish the diagnosis. Genetic counseling may help some couples and families learn about the risks and help with family planning. It also allows connecting patients with diseases registries and patient organizations. Some of the complications can be prevented with appropriate treatment. For example, a cardiac pacemaker or defibrillator can greatly reduce the risk for sudden death due to an abnormal heart rhythm. Physical therapy may be able to prevent or delay contractures and improve quality of life. Affected people may want to do DNA banking. DNA testing is recommended for those who are affected. This helps to identify the family gene mutation. Once the mutation is found, prenatal DNA testing, testing for carriers, and pre-implantation genetic diagnosis are possible. ReferencesBharucha-Goebel DX. Muscular dystrophies. In: Kliegman RM, St Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 627. Johnson NE, Statland JM. The limb-girdle muscular dystrophies. Continuum (Minneap Minn). 2022;28(6):1698-1714. PMID: 36537976 pubmed.ncbi.nlm.nih.gov/36537976/. Muscular Dystrophy Association website. Limb-girdle muscular dystrophy (LGMD). www.mda.org/disease/limb-girdle-muscular-dystrophy. Accessed March 5, 2024. Selcen D. Muscle diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 389. | ||
| ||
Review Date: 12/31/2023 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


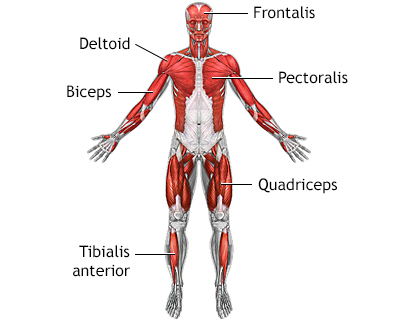 Superficial anteri...
Superficial anteri...
