Pregnancy SmartSiteTM
Myasthenic syndrome; Eaton-Lambert syndrome; Lambert-Eaton syndrome; LES DefinitionLambert-Eaton myasthenic syndrome (LEMS) is a rare disorder in which faulty communication between nerves and muscles leads to muscle weakness. CausesLEMS is an autoimmune disorder. This means your immune system mistakenly targets healthy cells and tissues in the body. With LEMS, antibodies produced by the immune system attack nerve cells. This makes nerves cells unable to release enough of a chemical called acetylcholine. This chemical transmits impulses between nerves and muscles. The result is muscle weakness. LEMS may occur with cancers such as small cell lung cancer or autoimmune disorders such as vitiligo, which leads to a loss of skin pigment. LEMS affects men more often than women. The most common age of occurrence is around age 60 years. LEMS is rare in children. SymptomsWeakness or loss of movement that can be more or less severe, including:
Weakness is generally mild in LEMS. Leg muscles are mostly affected. Weakness may improve after exercise, but continuous exertion causes fatigue in some cases. Symptoms related to the other parts of the nervous system often occur, and may include:
Exams and TestsYour health care provider will perform a physical exam and ask about your symptoms. The exam may show:
Tests to help diagnose and confirm LEMS may include:
A CT scan and an MRI of the chest and the abdomen, followed by bronchoscopy for smokers may be done to evaluate for cancer. PET scan may also be done if a lung tumor is suspected. You may be referred to an oncologist (cancer specialist) to determine if other cancer testing is needed. TreatmentThe main goals of treatment are to:
Plasma exchange, or plasmapheresis, is a treatment that helps remove from the body any harmful proteins (antibodies) that are interfering with nerve function. This involves removing blood plasma that contains the antibodies. Other proteins (such as albumin) or donated plasma are then infused into the body. Another procedure involves using intravenous immunoglobulin (IVIg) to infuse a large amount of helpful antibodies directly into the bloodstream. Medicines that may also be tried include:
Outlook (Prognosis)Symptoms of LEMS may improve by treating the underlying disease, suppressing the immune system, or removing the antibodies. However, paraneoplastic LEMS may not respond as well to treatment. (Paraneoplastic LEMS symptoms are due to an altered immune system response to a tumor). Death is due to underlying malignancy. Possible ComplicationsComplications of LEMS may include:
When to Contact a Medical ProfessionalContact your provider if symptoms of LEMS develop. ReferencesGuptill JT, Sanders DB. Disorders of neuromuscular transmission. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 108. Kaminski HJ. Disorders of neuromuscular transmission. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 390. Moss HE. Eyelid and facial nerve disorders. In: Liu GT, Volpe NJ, Galetta SL, eds. Liu, Volpe, and Galetta's Neuro-Ophthalmology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 14. | ||
| ||
Review Date: 6/13/2024 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


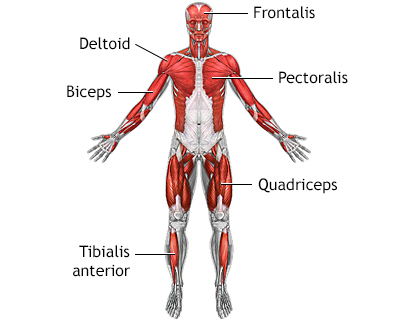 Superficial anteri...
Superficial anteri...
