Pregnancy SmartSiteTM
Acute sinusitis; Sinus infection; Sinusitis - acute; Sinusitis - chronic; Rhinosinusitis DefinitionSinusitis is present when the tissue lining the sinuses become swollen or inflamed. It occurs as the result of an inflammatory reaction or an infection from a virus, bacteria, or fungus. CausesThe sinuses are air-filled spaces in the skull. They are located behind the forehead, nasal bones, cheeks, and eyes. Most of the time, mucus is able to drain out and air is able to flow through the sinuses. When the sinus openings become blocked or too much mucus builds up, bacteria and other germs can grow more easily. Sinusitis can occur from one of these conditions:
There are three types of sinusitis:
The following may increase the risk that an adult or child will develop sinusitis:
SymptomsThe symptoms of acute sinusitis in adults very often follow a cold that does not get better or that gets worse after 7 to 10 days. Symptoms include:
Symptoms of chronic sinusitis are the same as those of acute sinusitis. However, the symptoms tend to be milder and last longer than 12 weeks. Symptoms of sinusitis in children include:
Exams and TestsThe health care provider will examine you or your child for sinusitis by:
The provider may view the sinuses through a fiberoptic scope (called nasal endoscopy or rhinoscopy) to diagnose sinusitis. This is often done by doctors who specialize in ear, nose, and throat problems (ENTs). Imaging tests that may be used to decide on treatment are:
Most of the time, regular x-rays of the sinuses do not diagnose sinusitis well. If you or your child has sinusitis that does not go away or keeps returning, other tests may include:
TreatmentSELF-CARE Try the following steps to reduce stuffiness in your sinuses:
Be careful with use of over-the-counter spray nasal decongestants such as oxymetazoline (Afrin) or phenylephrine (Neosynephrine). They may help at first, but using them for more than 3 to 5 days can make nasal stuffiness worse and lead to dependence. To help ease sinus pain or pressure:
MEDICINE AND OTHER TREATMENTS Most of the time, antibiotics are not needed for acute sinusitis. Most of these infections go away on their own. Even when antibiotics do help, they may only slightly reduce the time it takes for the infection to go away. Antibiotics are more likely to be prescribed sooner for:
Acute sinusitis should be treated for 5 to 10 days. Chronic sinusitis should be treated for 3 to 4 weeks. At some point, your provider will consider:
Other treatments for sinusitis include:
Surgery to enlarge the sinus opening and drain the sinuses may also be needed. You may consider this procedure if:
Most fungal sinus infections need surgery. Surgery to repair a deviated septum or nasal polyps may prevent the condition from returning. Outlook (Prognosis)Most sinus infections can be cured with self-care measures and medical treatment. If you are having repeated attacks, you should be checked for causes such as nasal polyps or other problems, such as allergies. Possible ComplicationsAlthough very rare, complications may include:
When to Contact a Medical ProfessionalContact your provider if:
A green or yellow discharge does not mean that you definitely have a sinus infection or need antibiotics. Many people with this symptom recover fully without taking antibiotics. PreventionThe best way to prevent sinusitis is to avoid colds and flu or treat problems quickly.
Other tips for preventing sinusitis:
ReferencesDeMuri GP, Wald ER. Sinusitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 62. Murr AH, Pletcher SD. Approach to the patient with nose, sinus, and ear disorders. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 394. Pappas DE, Boggs SR. Sinusitis. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 429. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1-S39. PMID: 25832968 pubmed.ncbi.nlm.nih.gov/25832968/. | ||
| ||
Review Date: 5/2/2024 Reviewed By: Josef Shargorodsky, MD, MPH, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


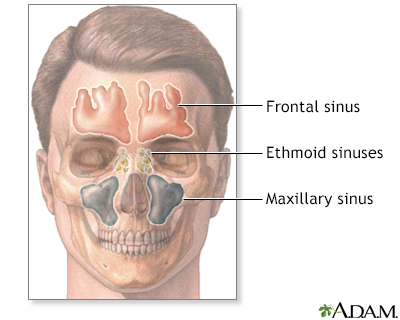 Sinuses
Sinuses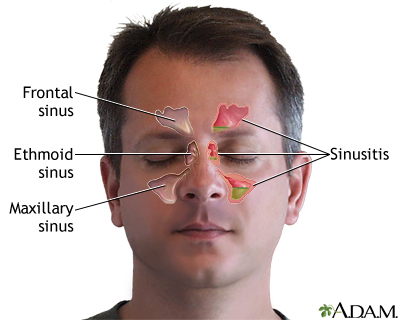 Sinusitis
Sinusitis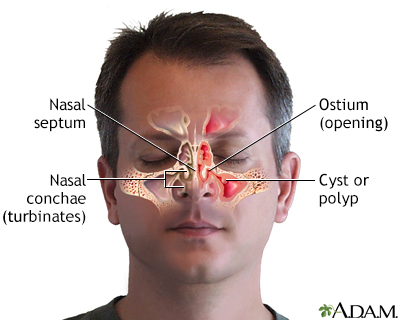 Chronic sinusitis
Chronic sinusitis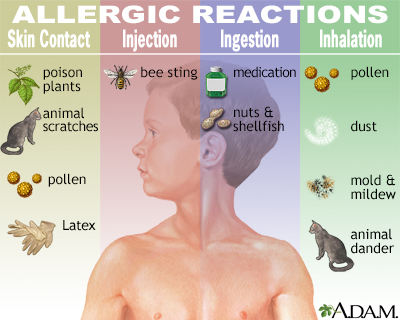 Allergic reactions
Allergic reactions
