Pregnancy SmartSiteTM
HIV infection; Infection - HIV; Human immunodeficiency virus; Acquired immune deficiency syndrome: HIV-1 DefinitionHuman immunodeficiency virus (HIV) is the virus that causes acquired immunodeficiency syndrome (AIDS). When a person becomes infected with HIV, the virus attacks and weakens the immune system. As the immune system weakens, the person is at risk for getting life-threatening infections and cancers. When that happens, the illness is called AIDS. Once a person has the virus, it stays inside the body for life. CausesThe virus is spread (transmitted) person-to-person through certain body fluids:
HIV can be spread if these fluids come in contact with:
HIV cannot be spread through sweat, saliva, or urine. In the United States, HIV is mainly spread:
Less often, HIV is spread:
The virus is not spread by:
HIV and blood or organ donation:
Risk factors for getting HIV include:
SymptomsSymptoms related to acute HIV infection (when a person is first infected) can be similar to the flu or other viral illnesses. They include:
Many people have no symptoms when they are first infected with HIV. Acute HIV infection (Stage 1) progresses over a few weeks to months to become chronic or asymptomatic HIV infection (Stage 2) (no symptoms). This stage can last 10 years or longer (not common). During this period, the person might have no reason to suspect they have HIV, but they can spread the virus to others. If they are not treated, almost all people infected with HIV will develop AIDS (Stage 3). Some people develop AIDS within a few years of infection. Others remain completely healthy after 10 or even 20 years (called long-term nonprogressors). People with AIDS have had their immune system seriously damaged by HIV. They are at very high risk of getting infections that are uncommon in people with a healthy immune system. These infections are called opportunistic infections and can affect any part of the body. These can be caused by:
People with AIDS are also at higher risk for certain cancers, especially lymphomas and a skin cancer called Kaposi sarcoma. Symptoms depend on the particular infection and which part of the body is infected. Lung infections are common in people with AIDS and often cause cough, fever, and shortness of breath. Intestinal infections are also common and can cause:
Other common symptoms in people with HIV infection and AIDS include:
Exams and TestsThere are tests that are done to check if you've been infected with HIV. DIAGNOSTIC TESTS In general, testing is a 2-step process:
Home tests are available to test for HIV. If you plan to use one, check to make sure it is approved by the FDA. Follow instructions on the packaging to ensure the results are as accurate as possible. The Centers for Disease Control and Prevention (CDC) recommends that everyone ages 15 to 65 have a screening test for HIV. People with risky behaviors should be tested regularly. Pregnant women should also have a screening test. TESTS AFTER BEING DIAGNOSED WITH HIV People with AIDS should have regular blood tests to check their CD4 cell count:
Other tests include:
All adults with HIV should have the following screening test for anal cancer:
Adults with HIV should have other tests along with high resolution anoscopy (HRA), rather than standard anoscopy, if they are:
If HRA is not available, people with HIV should continue to be screened using an assessment of symptoms and DARE. People with any symptoms or signs of anal cancer should have standard anoscopy, without the collection of anal specimens for diagnosis. TreatmentHIV/AIDS is treated with medicines that stop the virus from multiplying. This treatment is called antiretroviral therapy (ART). In the past, people with HIV infection would start antiretroviral treatment after their CD4 count dropped or they developed HIV complications. Today, HIV treatment is recommended for all people with HIV infection, even if their CD4 count is still normal. There are two types or treatment:
Regular blood tests are needed to make sure the virus level in the blood (viral load) is kept low or suppressed. The goal of treatment is to lower the HIV virus load in the blood to a level that is so low that the test can't detect it. This is called an undetectable viral load. If the CD4 count already dropped before treatment was started, it will usually slowly go up. HIV complications often disappear as the immune system recovers. Support GroupsJoining a support group where members share common experiences and problems can often help lower the emotional stress of having a long-term illness. Outlook (Prognosis)With treatment, most people with HIV/AIDS can live a healthy and normal life. Current treatments do not cure the infection. The medicines only work as long as they are taken every day or as prescribed. If the medicines are stopped, the viral load will go up and the CD4 count will drop. If the medicines are not taken regularly, the virus can become resistant to one or more of the medicines, and the treatment will stop working. People who are on treatment need to see their health care providers regularly. This is to make sure the medicines are working and to check for side effects of the medicines. When to Contact a Medical ProfessionalContact your provider for an appointment if you have any risk factors for HIV infection. Also contact your provider if you develop symptoms of AIDS. By law, the results of HIV testing must be kept confidential (private). Your provider will review your test results with you. PreventionPreventing HIV/AIDS:
Safer sex practices, such as using latex condoms, are effective in preventing the spread of HIV. But there is still a risk of getting the infection, even with the use of condoms (for example, condoms can tear). In people who aren't infected with the virus, but are at high risk of getting it, certain medicines can help prevent infection.
This treatment is known as pre-exposure prophylaxis, or PrEP. Talk to your provider if you think PrEP might be right for you. People who are HIV-positive, taking antiretroviral medicines, and have no detectible virus in their blood do not transmit the virus. The US blood supply is among the safest in the world. Nearly all people infected with HIV through blood transfusions received those transfusions before 1985, the year HIV testing began for all donated blood. If you believe you have been exposed to HIV, seek medical attention right away. Do not delay. Starting antiviral medicines right after the exposure (up to 3 days after) can reduce the chance that you will be infected. This is called post-exposure prophylaxis (PEP). It has been used to prevent transmission in health care workers injured by needlesticks. ReferencesCenters for Disease Control and Prevention website. HIV. About HIV. www.cdc.gov/hiv/about/index.html. Updated January 14, 2025. Accessed May 22, 2025. Centers for Disease Control and Prevention website. HIV. Preventing HIV with PrEP. www.cdc.gov/hiv/prevention/prep.html/. Reviewed January 18, 2024. Accessed May 22, 2025. Clinicalinfo.HIV.gov website. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/human. Reviewed January 8, 2025. Accessed July 17, 2025. Kleinpeter AP, Freed EO. Human immunodeficiency viruses. In: Blaser MJ, Cohen JI, Holland SM, et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 10th ed. Philadelphia, PA: Elsevier; 2026:chap 120. Merrick ST, Glesby MJ. Systemic manifestations of HIV/AIDS. Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 359. Peters C, Pham P, Maldarelli F. Diagnosis of human immunodeficiency virus infection. In: Blaser MJ, Cohen JI, Holland SM, et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 10th ed. Philadelphia, PA: Elsevier; 2026:chap 123. Tsibris AMN, Hirsch MS. Antiretroviral therapy for human immunodeficiency virus infection. In: Blaser MJ, Cohen JI, Holland SM, et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 10th ed. Philadelphia, PA: Elsevier; 2026:chap 130. US Department of Health and Human Services, Clinical Info HIV.gov website. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv/whats-new. Updated September 25, 2025. Accessed October 21, 2025. US Preventive Services Task Force, Owens DK, Davidson KW, Krist AH, et al. Screening for HIV Infection: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;321(23):2326-2336. PMID: 31184701 pubmed.ncbi.nlm.nih.gov/31184701/. | ||
| ||
Review Date: 5/12/2025 Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


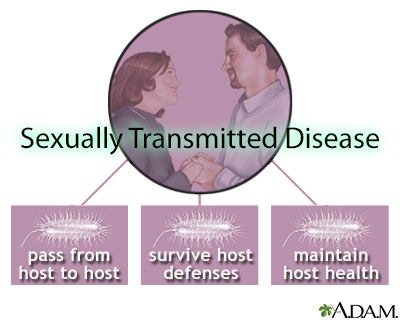 STDs and ecologica...
STDs and ecologica...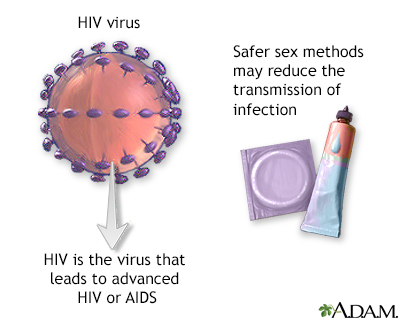 HIV
HIV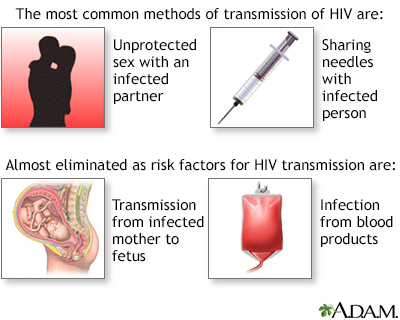 Primary HIV infect...
Primary HIV infect...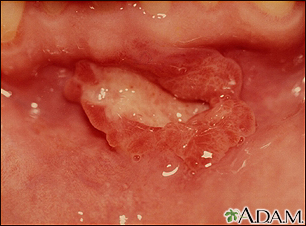 Canker sore (aphth...
Canker sore (aphth... Mycobacterium mari...
Mycobacterium mari... Dermatitis - sebor...
Dermatitis - sebor...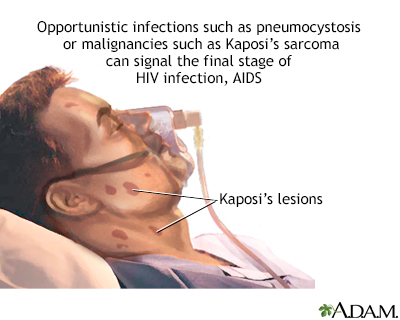 AIDS
AIDS Kaposi sarcoma - c...
Kaposi sarcoma - c... Histoplasmosis, di...
Histoplasmosis, di... Molluscum on the c...
Molluscum on the c...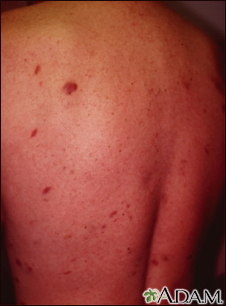 Kaposi sarcoma on ...
Kaposi sarcoma on ... Kaposi sarcoma on ...
Kaposi sarcoma on ... Molluscum contagio...
Molluscum contagio...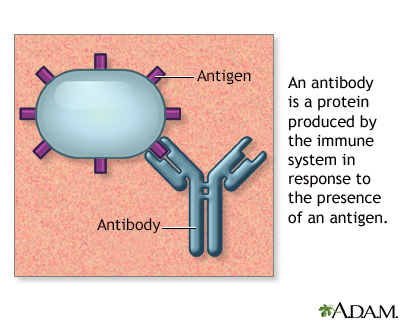 Antibodies
Antibodies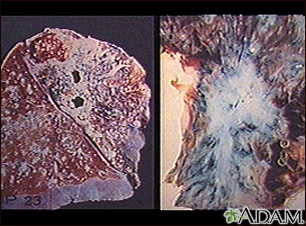 Tuberculosis in th...
Tuberculosis in th...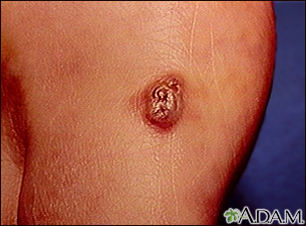 Kaposi sarcoma - l...
Kaposi sarcoma - l... Kaposi sarcoma - p...
Kaposi sarcoma - p... Herpes zoster (shi...
Herpes zoster (shi... Dermatitis seborrh...
Dermatitis seborrh...
