Pregnancy SmartSiteTM
Anticardiolipin antibodies; Hughes syndrome DefinitionAntiphospholipid syndrome (APS) is an autoimmune disorder that involves frequent blood clots (thromboses). When you have this condition, your body's immune system makes abnormal proteins that attack the blood cells and lining of the blood vessels. The presence of these antibodies can cause problems with blood flow and lead to dangerous clots in blood vessels throughout the body. CausesThe exact cause of APS is not known. Both certain gene changes and other factors (such as an infection) may cause the problem to develop. It is often found in people with other autoimmune diseases, such as systemic lupus erythematosus (SLE). The condition is more common in women than in men. It is often found in women who have a history of repeated miscarriages. Some people carry the antibodies mentioned above, but do not have APS. Certain triggers may cause these people to have a blood clot, including:
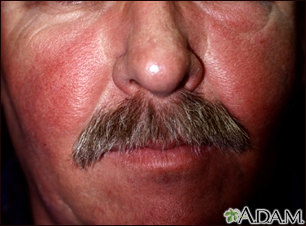
SymptomsYou may not have any symptoms, even though you have the antibodies. Symptoms that may occur include:
In rare cases, clots suddenly develop in many arteries over a period of days. This is called catastrophic anti-phospholipid syndrome (CAPS). It can lead to stroke as well as the clots in the kidney, liver, and other organs throughout the body, and gangrene in the limbs. CAPS has a high mortality rate, even with treatment. Exams and TestsTests for the lupus anticoagulant and antiphospholipid antibodies may be done when:
The lupus anticoagulant tests are blood clotting tests. The antiphospholipid antibodies (aPL) cause the test to be abnormal in the laboratory. Types of clotting tests may include:
Tests for antiphospholipid antibodies (aPL) will also be done. They include:
Your health care provider will diagnose APS if you have positive test for aPL or the lupus anticoagulant, and one or more of the following events:
The positive tests need to be confirmed after 12 weeks. If you have a positive test without other features of the disease, you will not have the diagnosis of APS. TreatmentThe treatment for APS is directed at preventing complications from new blood clots forming or existing clots getting larger. You will need to take some form of blood-thinning medicine. If you also have an autoimmune disease, such as lupus, you will need to keep that condition under control as well. The exact treatment will depend on how severe your condition is and the complications it is causing. ANTIPHOSPHOLIPID ANTIBODY SYNDROME (APS) In general, you will need treatment with a blood thinner for a long time if you have APS. Initial treatment may be heparin. This medicine is given by injection. In most cases, warfarin (Coumadin), which is given by mouth, is then started. It is necessary to frequently monitor the level of anticoagulation. This is most often done using the INR test. If you have APS and become pregnant, you will need to be followed closely by a provider who is an expert in this condition. You will not take warfarin during pregnancy, but will be given heparin shots instead. If you have SLE and APS, your provider may also recommend that you take hydroxychloroquine. Currently, other types of blood thinning medicines are not recommended. CATASTROPHIC ANTIPHOSPHOLIPID SYNDROME (CAPS) Treatment for CAPS that involves a combination of anticoagulation therapy, high doses of corticosteroids, and plasma exchange has been effective in most people. Sometimes IVIG, rituximab or eculizumab is also used for severe cases. POSITIVE TEST FOR LUPUS ANTICOAGULANT OR APL You will not need treatment if you do not have symptoms, pregnancy loss, or if you have never had a blood clot. Take the following steps to help prevent blood clots from forming:
You will be prescribed blood-thinning medicines (such as heparin and warfarin) to help prevent blood clots:
You may also need to take blood thinners for 3 to 4 weeks after surgery to lower your risk for blood clots. Outlook (Prognosis)Without treatment, people with APS will have repeat clotting events. Most of the time, outcome is good with proper treatment, which includes long-term anticoagulation therapy. Some people may have blood clots that are hard to control in spite of treatments. This can lead to CAPS, which can be life-threatening. When to Contact a Medical ProfessionalContact your provider if you notice symptoms of a blood clot, such as:
Also talk to your provider if you have repeated loss of pregnancy (miscarriage). Prevention
ReferencesBarbhaiya M, Salmon JE, Erkan D. Antiphospholipid syndrome. In: Firestein GS, McInnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelly's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 83. Cervera R, Rodriguez-Pinto I, Leagult K, Erkan D. 16th International Congress on Antiphospholipid Antibodies Task Force Report on catastrophic antiphospholipid syndrome. Lupus. 2020:29(12):1594-1600. PMID 32819183 pubmed.ncbi.nlm.nih.gov/32819183/. National Heart, Lung, and Blood Institute website. Antiphospholipid syndrome (APS). www.nhlbi.nih.gov/health/antiphospholipid-syndrome. Updated March 24, 2022. Accessed February 19, 2025. | ||
| ||
Review Date: 1/28/2025 Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Systemic lupus ery...
Systemic lupus ery...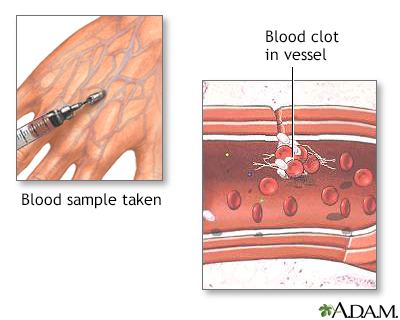 Blood clots
Blood clots
