Pregnancy SmartSiteTM
Transitional cell carcinoma of the bladder; Urothelial cancer DefinitionBladder cancer is a cancer that starts in the bladder. The bladder is the body part that holds and releases urine. It is in the center of the lower abdomen. CausesBladder cancer often starts from the cells lining the bladder. These cells are called transitional cells. These tumors are classified by the way they grow:
The exact cause of bladder cancer is not known. But several things that may make you more likely to develop it include:
Research has not shown clear evidence that using artificial sweeteners leads to bladder cancer in humans. SymptomsSymptoms of bladder cancer can include:
Other diseases and conditions can cause similar symptoms. It is important to see your health care provider to check for all other possible causes. Exams and TestsThe provider will perform a physical examination, including a rectal and pelvic exam. Tests that may be done include:
If tests confirm you have bladder cancer, additional tests will be done to see if the cancer has spread. This is called staging. Staging helps guide future treatment and follow-up and gives you some idea of what to expect in the future. The TNM (tumor, nodes, metastasis) staging system is used to stage bladder cancer:
Tumors are also grouped based on how they appear under a microscope. This is called grading the tumor. A high-grade tumor is fast growing and more likely to spread. Bladder cancer can spread into nearby areas, including the:
TreatmentTreatment depends on the stage of the cancer, the severity of your symptoms, and your overall health. Stage 0 and I treatments:
Stage II and III treatments:
Most people with stage IV tumors cannot be cured and surgery is not appropriate. In these people, chemotherapy, the antibody-drug conjugate enfortumab vedotin (Padcev), targered therapy, and immunotherapy are often considered. CHEMOTHERAPY Chemotherapy may be given to people with stage II and III disease either before or after surgery to help prevent the tumor from returning. For early disease (stages 0 and I), chemotherapy is usually given directly into the bladder. IMMUNOTHERAPY Bladder cancers are often treated with immunotherapy. In this treatment, a medicine triggers your immune system to attack and kill the cancer cells. Immunotherapy for early stage bladder cancer is often performed using the Bacille Calmette-Guerin vaccine (commonly known as BCG). If the cancer returns after the use of BCG, newer agents may be used. As with all treatments, side effects are possible. Ask your provider what side effects you might expect, and what to do if they occur. SURGERY Surgery for bladder cancer includes:
Surgery may also be done to help your body drain urine after the bladder is removed. This may include:
Support GroupsYou can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone. Outlook (Prognosis)After treatment for bladder cancer, you will be closely monitored by a provider. This may include:
How well a person with bladder cancer does depends on the initial stage and response to treatment of the bladder cancer. The outlook for stage 0 or I cancers is fairly good. Although the risk for the cancer returning is high, most bladder cancers that return can be surgically removed and cured. The cure rates for people with stage III tumors are less than 50%. People with stage IV bladder cancer are rarely cured. Possible ComplicationsBladder cancers may spread into the nearby organs. They may also travel through the pelvic lymph nodes and spread to the liver, lungs, and bones. Additional complications of bladder cancer include:
When to Contact a Medical ProfessionalContact your provider if you have blood in your urine or other symptoms of bladder cancer, including:
PreventionIf you smoke, quit. Smoking can increase your risk for bladder cancer. Avoid exposure to chemicals linked to bladder cancer. ReferencesNational Cancer Institute website. Bladder cancer treatment (PDQ) - health professional version. www.cancer.gov/types/bladder/hp/bladder-treatment-pdq. Updated January 18, 2023. Accessed May 6, 2024. National Comprehensive Cancer Network website. NCCN guidelines for patients: Bladder cancer. Version 4.2023. www.nccn.org/patients/guidelines/content/PDF/bladder-patient.pdf. Accessed May 6, 2024. Smith AB, Balar AV, Milowsky MI, Chen RC. Carcinoma of the bladder. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 80. | ||
| ||
Review Date: 3/31/2024 Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


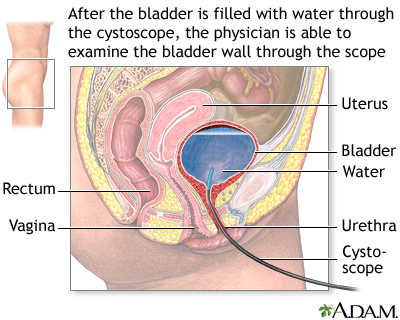 Cystoscopy
Cystoscopy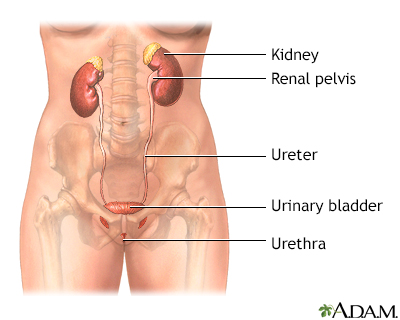 Female urinary tra...
Female urinary tra... Male urinary tract
Male urinary tract
