Pregnancy SmartSiteTM
Patellofemoral syndrome; Chondromalacia patella; Runner's knee; Patellar tendinitis; Jumper's knee DefinitionAnterior knee pain is pain that occurs at the front and center of the knee. It can be caused by many different problems, including:
CausesYour kneecap (patella) sits over the front of your knee joint. As you bend or straighten your knee, the underside of the patella glides over the bones that make up the knee. Strong tendons help attach the kneecap to the bones and muscles that surround the knee. These tendons are called:
Anterior knee pain may occur when the kneecap does not move properly and rubs against the lower part of the thigh bone. This may occur because:
Anterior knee pain is more common in:
Other possible causes of anterior knee pain include:
SymptomsAnterior knee pain is a dull, aching pain that is most often felt in one or more location:
One common symptom is a grating or grinding feeling when the knee is flexed (when the ankle is brought closer to the back of the thigh). Symptoms may be more noticeable with:
Exams and TestsYour health care provider will perform a physical exam. The knee may be tender and mildly swollen. Also, the kneecap may not be perfectly lined up with the thigh bone (femur). When you flex your knee, you may feel a grinding feeling below the kneecap. Pressing the kneecap when the knee is straightening out may be painful. Your provider may want you to do a single leg squat to look at muscle imbalance and your core stability. X-rays are very often normal. However, a special x-ray view of the kneecap may show signs of arthritis or tilting. MRI scans are rarely needed. TreatmentResting the knee for a short period of time and taking nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, or aspirin may help relieve pain. Other things you can do to relieve anterior knee pain include:
Rarely, surgery for pain behind the kneecap is needed. During the surgery:
Outlook (Prognosis)Anterior knee pain often improves with a change in activity, exercise therapy, and the use of NSAIDs. Surgery is rarely needed. However, if your knee has symptoms like instability or swelling, then you should see your provider earlier. When to Contact a Medical ProfessionalContact your provider if you have symptoms of this disorder. ReferencesDeJour D, Saggin PRF, Kuhn VC. Disorders of the patellofemoral joint. In: Scott WN, ed. Insall & Scott Surgery of the Knee. 6th ed. Philadelphia, PA: Elsevier; 2018:chap 65. Huntoon E, DEC Louise K, Caldwell M. Lower limb pain and dysfunction. In: Cifu DX, ed. Braddom's Physical Medicine Rehabilitation. 6th ed. Philadelphia, PA: Elsevier; 2021:chap 36. McCarthyM, McCarty EC, Frank RM. Patellofemoral pain. In: Miller MD, Thompson SR, eds. DeLee, Drez, & Miller's Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 106. Teitge RA. Patellofemoral disorders: correction of rotational malalignment of the lower extremity. In: Noyes FR, Barber-Westin SD, eds. Noyes' Knee Disorders: Surgery, Rehabilitation, Clinical Outcomes. 2nd ed. Philadelphia, PA: Elsevier; 2017:chap 36. Wilson H, Middleton R, Price AJ. The knee. In: Hochberg MC, Gravallese EM, Smolen JS, van der Heijde D, Weinblatt ME, Weisman MH, eds. Rheumatology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 83. | ||
| ||
Review Date: 10/15/2023 Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


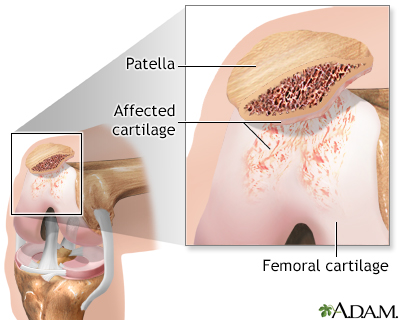 Chondromalacia of ...
Chondromalacia of ...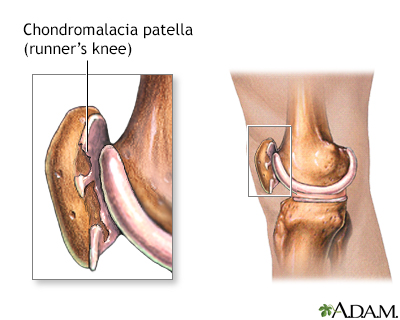 Runners knee
Runners knee
