Pregnancy SmartSiteTM
Arteritis - temporal; Cranial arteritis; GCA DefinitionGiant cell arteritis (GCA) is inflammation and damage to the blood vessels that supply blood to the head, neck, upper body and arms. It is also called temporal arteritis. CausesGiant cell arteritis affects medium-to-large arteries. It causes inflammation, swelling, tenderness, and damage to the blood vessels that supply blood to the head, neck, upper body, and arms. It most commonly occurs in the arteries around the temples (temporal arteries). These arteries branch off from the carotid artery in the neck. In some cases, the condition can occur in medium-to-large arteries in other places in the body as well. The cause of the condition is unknown. It is believed to be due in part to a faulty immune response. The disorder has been linked to some infections and to certain genes. Giant cell arteritis is more common in people with another inflammatory disorder known as polymyalgia rheumatica. While GCA is a considerably uncommon condition, it primarily affects individuals over the age of 50. It is most common in people of northern European descent. The condition may run in families. SymptomsSome common symptoms of this problem are:
Other symptoms may include:
Problems with eyesight may occur, and at times may begin suddenly. These problems include:
Exams and TestsThe health care provider will examine your head.
Blood tests may include:
Blood tests alone cannot provide a diagnosis. You may need to have a biopsy of the temporal artery. This is a surgical procedure that can be done as an outpatient. You may also have other tests, including:
TreatmentGetting prompt treatment can help prevent severe problems such as blindness or stroke. When giant cell arteritis is suspected, you will receive corticosteroids, such as prednisone, by mouth. These medicines are often started even before a biopsy is done. You may also be told to take aspirin. Most people begin to feel better within a few days after starting treatment. The dose of corticosteroids will be cut back very slowly. However, you will need to take medicine for 1 to 2 years. If the diagnosis of giant cell arteritis is made, in most people a biologic medicine called tocilizumab will be added. This medicine reduces the amount of corticosteroids needed to control the disease. Long-term treatment with corticosteroids can make bones thinner and increase your chance of a fracture. You will need to take the following steps to protect your bone strength.
Outlook (Prognosis)Most people make a full recovery, but treatment may be needed for 1 to 2 years or longer. The condition may return at a later date. Damage to other blood vessels in the body, such as aneurysms (ballooning of the blood vessels), may occur. This damage can lead to a stroke in the future. When to Contact a Medical ProfessionalContact your provider if you have:
You may be referred to a specialist who treats temporal arteritis. PreventionThere is no known prevention. ReferencesAmerican College of Rheumatology website. Giant cell arteritis. rheumatology.org/patients/giant-cell-arteritis. Updated February 2025. Accessed March 24, 2025. Antonio AA, Santos RN, Abariga SA. Tocilizumab for giant cell arteritis. Cochrane Database Syst Rev. 2022;5(5):CD013484. PMID: 35560150 pubmed.ncbi.nlm.nih.gov/35560150/. James WD. Cutaneous vascular diseases. In: James WD, ed. Andrews' Diseases of the Skin: Clinical Dermatology. 14th ed. Philadelphia, PA: Elsevier; 2026:chap 30. Miller JB, Hellmann DB. Giant cell arteritis, polymyalgia rheumatica, and Takayasu's arteritis. In: Firestein GS, Mclnnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 89. Spiera R. Giant cell arteritis and polymyalgia rheumatica. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 250. Stone JH, Han J, Aringer M, et al. Long-term effect of tocilizumab in patients with giant cell arteritis: open-label extension phase of the Giant Cell Arteritis Actemra (GiACTA) trial. Lancet Rheumatol. 2021;3(5):e328-e336. PMID: 38279390 pubmed.ncbi.nlm.nih.gov/38279390/. | ||
| ||
Review Date: 1/28/2025 Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


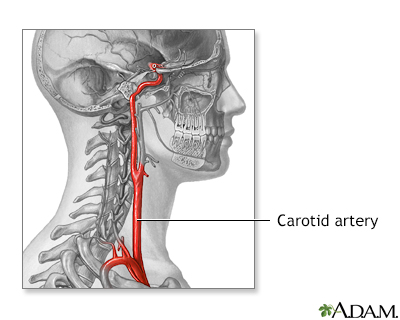 Carotid artery ana...
Carotid artery ana...
