Pregnancy SmartSiteTM
DefinitionNecrotizing vasculitis is a group of disorders that involve inflammation of the blood vessel walls. The size of the affected blood vessels helps to determine the names of these conditions and how the disorder causes disease. CausesNecrotizing vasculitis may be the primary condition such as in people with polyarteritis nodosa or granulomatosis with ANCA associated vasculitis (formerly called Wegener granulomatosis). In other cases, the vasculitis may occur as part of another disorder, such as systemic lupus erythematosus or hepatitis C. The cause of the inflammation is unknown. It is likely related to autoimmune factors. The wall of the blood vessel may scar and thicken or die (become necrotic). The blood vessel may close, interrupting blood flow to the tissues it supplies. The lack of blood flow will cause the tissues to die. Sometimes the blood vessel may break and bleed (rupture). Necrotizing vasculitis may affect blood vessels in any part of the body. Therefore, it can cause problems in the skin, brain, lungs, intestines, kidney, brain, joints or any other organ. SymptomsFever, chills, fatigue, arthritis, or weight loss may be the only symptoms at first. However, symptoms may be in almost any part of the body. Skin:
Muscles and joints:
Brain and nervous system:
Lungs and respiratory tract:
Other symptoms include:
Exams and TestsThe health care provider will do a complete physical exam. A nervous system (neurological) exam may show signs of nerve damage. Tests that may be done include:
TreatmentCorticosteroids are given in most cases. The dose will depend on how bad the condition is. Other medicines that suppress the immune system may reduce inflammation of the blood vessels. These include azathioprine, methotrexate, and mycophenolate. These medicines are often used along with corticosteroids. This combination makes it possible to control the disease with a lower dose of corticosteroids. For severe disease, cyclophosphamide (Cytoxan) has been used for many years. However, rituximab (Rituxan) is equally effective and is less toxic. Recently, tocilizumab (Actemra) was shown to be effective for giant cell arteritis so the dose of corticosteroids could be reduced. Outlook (Prognosis)Necrotizing vasculitis can be serious and life-threatening disease. The outcome depends on the location of the vasculitis and the severity of tissue damage. Complications may occur from the disease and from the medicines. Most forms of necrotizing vasculitis require long-term follow-up and treatment. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalContact your provider if you have symptoms of necrotizing vasculitis. Emergency symptoms include:
PreventionThere is no known way to prevent this disorder. ReferencesChung SA, Monach PA. Anti-neutrophil cytoplasmic antibody–associated vasculitis. In: Firestein GS, McInnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 90. Dinulos JGH. Hypersensitivity syndromes and vasculitis. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 18. Free M, Jennette JC, Falk RJ, Jain K. Renal and systemic vasculitis. In: Johnson RJ, Floege J, Tonelli M, eds. Comprehensive Clinical Nephrology. 7th ed. Philadelphia, PA: Elsevier; 2024:chap 26. Rhee RL, Merkel PA. Classification and epidemiology of systemic vasculitis. In: Firestein GS, McInnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 88. Stone JH. The systemic vasculitides. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 249. | ||
| ||
Review Date: 4/1/2025 Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


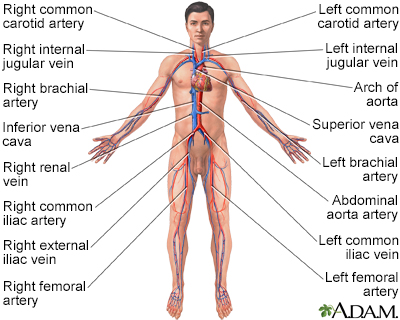 Circulatory system
Circulatory system
