Pregnancy SmartSiteTM
Progressive systemic sclerosis; Systemic sclerosis; Limited scleroderma; CREST syndrome; Localized scleroderma; Morphea - linear; Raynaud's phenomenon - scleroderma DefinitionScleroderma is a disease that involves the buildup of fibrous tissue in the skin and elsewhere in the body. It also damages the cells that line the walls of small arteries. This leads to tissue injury due to poor blood supply. CausesScleroderma is a type of autoimmune disorder. In this condition, the immune system mistakenly attacks and damages healthy body tissue. The cause of scleroderma is unknown. A buildup of a protein normally found in the body (called collagen) in the skin and other organs leads to the symptoms of the disease. The disease most often affects people ages 30 to 50 years. Women get scleroderma more often than men. Some people with scleroderma have a history of being around silica dust and polyvinyl chloride, but most do not. Widespread scleroderma can occur with other autoimmune diseases, including systemic lupus erythematosus and polymyositis. These cases are referred to as undifferentiated connective tissue disease or overlap syndrome. SymptomsSome types of scleroderma affect only the skin, while others affect the whole body.
Skin signs of scleroderma may include:
Bone and muscle symptoms may include:
Breathing problems may result from scarring in the lungs and can include:
Digestive tract problems may include:
Heart problems may include:
Kidney and genitourinary problems may include:
Exams and TestsThe health care provider will do a complete physical exam. The exam may show:
Your blood pressure will be checked. Scleroderma can cause small blood vessels in the kidneys to become narrowed. Problems with your kidneys can lead to high blood pressure and decrease function of the kidney. Blood and urine tests may include:
Other tests may include:
TreatmentThere is no specific treatment for scleroderma. Your provider will assess the extent of disease in the skin, lungs, kidneys, heart, and gastrointestinal tract. People with diffuse skin disease (rather than limited skin involvement) may be more prone to progressive and internal organ disease. This form of the disease is classified as diffuse cutaneous systemic sclerosis (dcSSc). Body wide (systemic) treatments are most often used for this group of patients. You will be prescribed medicines and other treatments to control your symptoms and prevent complications. Medicines used to treat progressive scleroderma include:
Some people with rapidly progressive scleroderma may be candidates for autologous hematopoietic stem cell transplantation (HSCT). This type of treatment needs to be performed in specialized centers. Other treatments for specific symptoms may include:
Treatment often involves physical therapy as well. Support GroupsSome people can benefit from attending a support group for people with scleroderma. Outlook (Prognosis)In some people, symptoms develop quickly for the first few years and continue to get worse. However, in most people, the disease gets worse only slowly. People who have only skin symptoms have a better outlook. Widespread (systemic) scleroderma can lead to.
When to Contact a Medical ProfessionalContact your provider if you develop Raynaud phenomenon, progressive thickening of the skin, or trouble swallowing. Prevention
ReferencesHerrick AL, Pan X, Peytrignet S, et al. Treatment outcome in early diffuse cutaneous systemic sclerosis: the European Scleroderma Observational Study (ESOS). Ann Rheum Dis. 2017;76(7):1207-1218. PMID: 28188239 pubmed.ncbi.nlm.nih.gov/28188239/. Poole JL, Dodge C. Scleroderma: therapy. In: Skirven TM, Osterman AL, Fedroczyk JM, Amadio PC, Feldscher SB, Shin EK, eds. Rehabilitation of the Hand and Upper Extremity. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 92. Sullivan KM, Goldmuntz EA, Keyes-Elstein L, et al. Myeloablative autologous stem-cell transplantation for severe scleroderma. N Engl J Med. 2018;378(1):35-47. PMID: 29298160 pubmed.ncbi.nlm.nih.gov/29298160/. Varga J. Etiology and pathogenesis of systemic sclerosis. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 88. Varga J. Systemic sclerosis (scleroderma). In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 246. | ||
| ||
Review Date: 5/9/2024 Reviewed By: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, NY and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


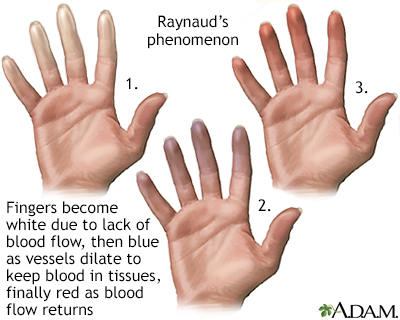 Raynaud's phenomen...
Raynaud's phenomen...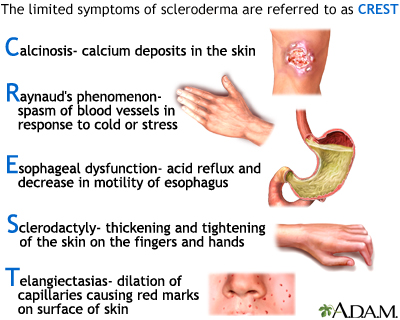 CREST syndrome
CREST syndrome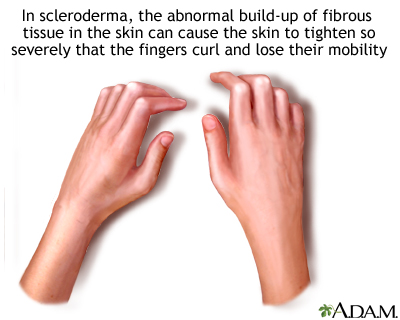 Sclerodactyly
Sclerodactyly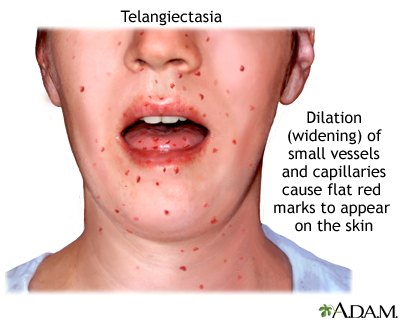 Telangiectasia
Telangiectasia
