Pregnancy SmartSiteTM
DefinitionPolymyositis and dermatomyositis are rare inflammatory diseases. These diseases lead to muscle weakness, swelling, tenderness, and tissue damage. They are part of a larger group of diseases called myopathies, more specifically inflammatory myopathies. CausesPolymyositis affects the skeletal muscles. It is also known as idiopathic inflammatory myopathy. The exact cause is unknown, but it may be related to an autoimmune reaction or infection. Polymyositis can affect people at any age. It is most common in adults between ages 50 and 60, and in older children. It affects women twice as often as men. It is more common in African Americans than white people. SymptomsPolymyositis is a systemic disease. This means it affects the whole body. Muscle weakness and tenderness can be signs of polymyositis. A rash is a sign of a related condition, dermatomyositis. Common symptoms include:
You may also have:
Exams and TestsTests may include:
People with this condition also must be watched carefully for signs of cancer. TreatmentThe initial treatment is the use of corticosteroid medicines. The dose of medicine is slowly tapered off as muscle strength improves. Medicines to suppress the immune system may be used to replace the corticosteroids. These medicines may include azathioprine, methotrexate, rituximab (Rituxan), or mycophenolate. For disease that remains active in spite of corticosteroids, intravenous gamma globulin can be given. It is important to check for other conditions in people who do not respond to treatment. A repeat muscle biopsy may be needed to make this diagnosis. If the condition is associated with a tumor, it may improve if the tumor is removed. Outlook (Prognosis)Response to treatment varies, based on the complications. As many as 1 in 5 people may die within 5 years of developing the condition. Many people, especially children, recover from the illness and do not need ongoing treatment. For most adults, however, immunosuppressant medicines are needed to control the disease. The outlook for people with lung disease with the anti-MDA-5 antibody is poor despite current treatment. In adults, death may result from:
The major causes of death are cancer and lung disease. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalContact your health care provider if you have symptoms of this disorder. Seek emergency treatment if you have shortness of breath and difficulty swallowing. ReferencesGreenberg SA. Inflammatory myopathies. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 248. Nagaraju K, Aggarwal R, Lundberg IE. Inflammatory diseases of muscle and other myopathies In: Firestein GS, Mclnnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 86. National Organization for Rare Disorders website. Polymyositis and necrotizing myopathy. rarediseases.org/rare-diseases/polymyositis/. Updated August 26, 2019. Accessed March 24, 2025. | ||
| ||
Review Date: 1/28/2025 Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


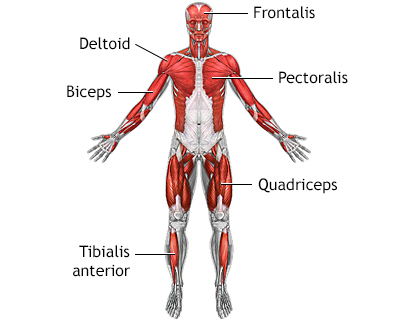 Superficial anteri...
Superficial anteri...
