Pregnancy SmartSiteTM
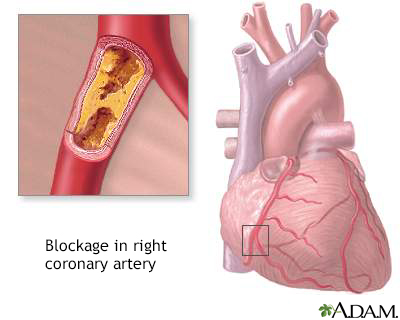
Multiple lipoprotein-type hyperlipidemia DefinitionFamilial combined hyperlipidemia is a disorder that is passed down through families. It causes high blood cholesterol and triglyceride levels. CausesFamilial combined hyperlipidemia is the most common genetic disorder that increases blood fats. It can cause early heart attacks. Diabetes, alcohol use, and hypothyroidism make the condition worse. Risk factors for being diagnosed with this condition include a family history of high cholesterol and early coronary artery disease. SymptomsIn the early years, there may be no symptoms. When symptoms appear, they may be due to impaired blood flow to parts of the body and include:
People with this condition may develop high cholesterol or triglyceride levels as teenagers. The condition may also be diagnosed when people are in their 20s and 30s. The levels remain high all during life. Those with familial combined hyperlipidemia have an increased risk of early coronary artery disease and heart attacks. They also have higher rates of obesity and are more likely to have glucose intolerance. Exams and TestsBlood tests will be done to check your levels of cholesterol and triglycerides. Tests will show:
Genetic testing is available for one type of familial combined hyperlipidemia. TreatmentThe goal of treatment is to reduce the risk of atherosclerotic heart disease. LIFESTYLE CHANGES The first step is to change what you eat. Most of the time, you will try diet changes for several months before your health care provider recommends medicines. Diet changes include lowering the amount of saturated fat and refined sugar. Here are some changes you can make:
It may help to talk to a dietitian who can give you advice about changing your eating habits. Weight loss and regular exercise may also help lower your cholesterol level. MEDICINES If lifestyle changes do not change your cholesterol levels enough, or you are at very high risk for atherosclerotic heart disease, your provider may recommend that you take medicines. There are several types of medicines to help lower blood cholesterol levels. The medicines work in different ways to help you achieve healthy lipid levels. Some are better at lowering LDL cholesterol, some are good at lowering triglycerides, while others help raise HDL cholesterol. The most commonly used, and most effective medicines for treating high LDL cholesterol are called statins. They include lovastatin (Mevacor), pravastatin (Pravachol), simvastatin (Zocor), fluvastatin (Lescol), atorvastatin (Lipitor), rosuvastatin (Crestor), and pitivastatin (Livalo). Other cholesterol-lowering medicines include:
Outlook (Prognosis)How well you do depends on:
Without treatment, heart attack or stroke may cause early death. Even with medicine, some people may continue to have high lipid levels that increase their risk for heart attack. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalSeek medical care right away if you have chest pain or other warning signs of a heart attack. Contact your provider if you have a personal or family history of high cholesterol levels. PreventionA diet that is low in cholesterol and saturated fat may help to control LDL levels in people at high risk. If someone in your family has this condition, you may want to consider genetic screening for yourself or your children. Sometimes, younger children may have mild hyperlipidemia. It is important to control other risk factors for early heart attacks, such as smoking. ReferencesGenest J, Mora S, Libby P. Lipoprotein disorders and cardiovascular disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 27. Robinson JG. Disorders of lipid metabolism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 190. | ||
| ||
Review Date: 5/8/2024 Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Coronary artery bl...
Coronary artery bl... Healthy diet
Healthy diet
