Pregnancy SmartSiteTM
De Quervain's thyroiditis; Subacute nonsuppurative thyroiditis; Giant cell thyroiditis; Subacute granulomatous thyroiditis; Hyperthyroidism - subacute thyroiditis DefinitionSubacute thyroiditis is an immune reaction of the thyroid gland that often follows an upper respiratory infection. The thyroid gland is located in the neck, just above where your collarbones meet in the middle. CausesSubacute thyroiditis is an uncommon condition. It is thought to be the result of a viral infection. The condition often occurs a few weeks after a viral infection of the ear, sinus, or throat, such as mumps, the flu, or a common cold. Subacute thyroiditis occurs most often in middle-aged women with symptoms of a viral upper respiratory tract infection in the past month. SymptomsThe most obvious symptom of subacute thyroiditis is pain in the neck caused by a swollen and inflamed thyroid gland. Sometimes, the pain can spread (radiate) to the jaw or ears. The thyroid gland may be painful and swollen for weeks or, in rare cases, months. Other symptoms include:
The inflamed thyroid gland may release too much thyroid hormone, causing symptoms of hyperthyroidism, including:
As the thyroid gland heals, it may release too little hormone, causing symptoms of hypothyroidism, including:
Thyroid gland function often returns to normal over a few months. During this time you may need treatment for your underactive thyroid. In rare cases, hypothyroidism may be permanent. Exams and TestsLaboratory tests that may be done include:
TreatmentThe goal of treatment is to reduce pain and treat hyperthyroidism, if it occurs. Medicines such as aspirin or ibuprofen are used to control pain in mild cases. More serious cases may need short-term treatment with medicines that reduce swelling and inflammation, such as prednisone. Symptoms of an overactive thyroid are treated with a class of medicines called beta-blockers. If the thyroid becomes underactive during the recovery phase, thyroid hormone replacement may be needed. Outlook (Prognosis)The condition should improve on its own. But the illness may last for months. Long-term or severe complications do not often occur. The condition is not infectious. People cannot catch it from you. It is not inherited within families like some thyroid conditions. When to Contact a Medical ProfessionalContact your health care provider if:
PreventionVaccines that prevent viral infections such as the flu may help prevent subacute thyroiditis. Other causes may not be preventable. ReferencesBrent GA, Weetman AP. Hypothyroidism and thyroiditis. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 13. Hollenberg A, Wiersinga WM. Hyperthyroid disorders. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 12. Pearce EN, Hollenberg AN. Thyroid. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 207. Ramos-Levi AM, Marazuela M. Thyroiditis. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 73. Smith JR, Wassner AJ. Thyroiditis. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 582. | ||
| ||
Review Date: 2/28/2024 Reviewed By: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


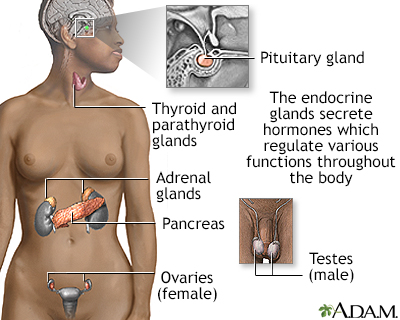 Endocrine glands
Endocrine glands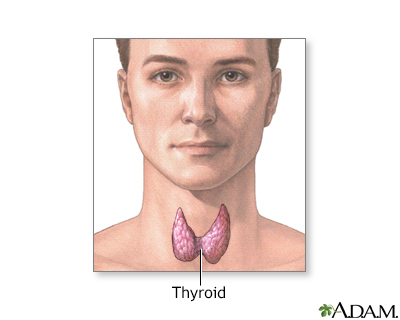 Thyroid gland
Thyroid gland
