Pregnancy SmartSiteTM
Pituitary insufficiency; Panhypopituitarism DefinitionHypopituitarism is a condition in which the pituitary gland does not produce normal amounts of some or all of its hormones. CausesThe pituitary gland is a small structure that is located just below the brain. It is attached by a stalk to the hypothalamus. The hypothalamus is the area of the brain that regulates the pituitary gland's function. The hormones released by the pituitary gland (and their functions) are:
In hypopituitarism, there is a lack of one or more pituitary hormones. Lack of a hormone leads to loss of function in the gland or organ the hormone regulates. For example, lack of TSH leads to loss of normal function of the thyroid gland. Hypopituitarism may be caused by:
Sometimes, hypopituitarism is due to uncommon immune system or metabolic diseases, such as:
Hypopituitarism is also a rare complication caused by severe bleeding during pregnancy. The loss of blood leads to tissue death in the pituitary gland. This condition is called Sheehan syndrome. Certain medicines can also suppress pituitary function. The most common medicines are glucocorticoids (such as prednisone and dexamethasone), which are taken for inflammatory and immune conditions. Medicines used to treat prostate cancer can also lead to low pituitary function. SymptomsSymptoms of hypopituitarism include any of the following (multiple symptoms are common):
Symptoms may develop slowly and may vary greatly, depending upon:
Other symptoms that may occur with this condition: Exams and TestsTo diagnose hypopituitarism, there must be low hormone levels due to a problem with the pituitary gland. The diagnosis must also check for diseases of the organ that is affected by this hormone. Tests may include:
The level of a pituitary hormone may be high in the bloodstream if you have a pituitary tumor that is producing too much of that hormone. The tumor may compress other cells of the pituitary, leading to low levels of other hormones. TreatmentIf hypopituitarism is caused by a tumor, you may need surgery to remove the tumor. Radiation therapy may also be needed. You will need lifelong hormone medicines to replace hormones that are no longer made by organs under the control of the pituitary gland. These may include:
Medicines are also available to treat related infertility in men and women. If you take glucocorticoid medicines for pituitary ACTH deficiency, be sure you know when to take a stress dose of your medicine. Discuss this with your health care provider. Always carry a medical ID (card, bracelet, or necklace) that says you have adrenal insufficiency. The ID should also say the type of medicine and dosage you need in case of an emergency caused by adrenal insufficiency. Outlook (Prognosis)Hypopituitarism is usually permanent. It requires lifelong treatment with one or more medicines. But you can expect a normal life span. In children, hypopituitarism due to a tumor may improve if the tumor is removed by surgery. Possible ComplicationsSide effects of medicines to treat hypopituitarism can develop. However, do not stop any medicine on your own without talking with your provider first. When to Contact a Medical ProfessionalContact your provider if you develop symptoms of hypopituitarism. PreventionIn most cases, the disorder is not preventable. Awareness of risk, such as from taking certain medicines, may allow early diagnosis and treatment. ReferencesClemmons DR, Nieman LK. Approach to the patient with endocrine disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 202. Fleseriu M, Hashim IA, Karavitaki N, et al. Hormonal replacement in hypopituitarism in adults: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(11):3888-3921. PMID: 27736313 pubmed.ncbi.nlm.nih.gov/27736313/. Johannsson G, Ragnarsson O. Hypopituitarism including growth hormone deficiency. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 5. Kaiser U, Ho KKY. Pituitary physiology and diagnostic evaluation. In: Melmed S, Auchus RJ, Goldfine AB, Rosen CJ, Kopp PA, eds. Williams Textbook of Endocrinology. 15th ed. Philadelphia, PA: Elsevier; 2025:chap 6. Weiss RE. Anterior pituitary. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 205. | ||
| ||
Review Date: 4/24/2025 Reviewed By: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


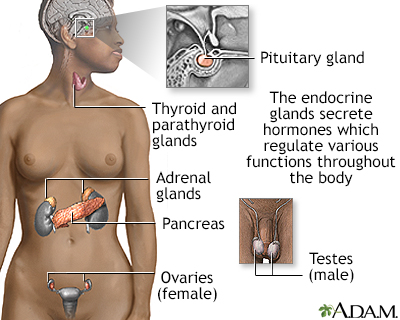 Endocrine glands
Endocrine glands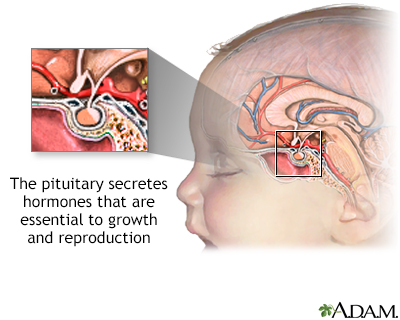 The pituitary glan
The pituitary glan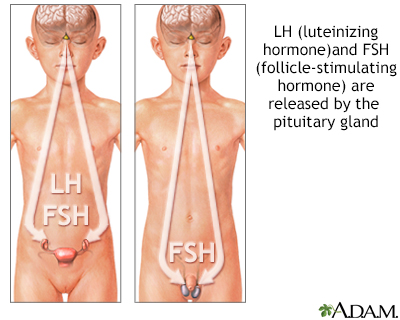 Gonadotropins
Gonadotropins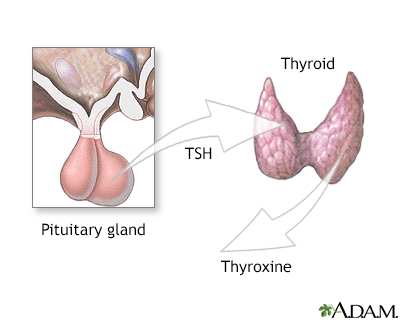 Pituitary and TSH
Pituitary and TSH
