Pregnancy SmartSiteTM
Type 2 diabetes - managing DescriptionType 2 diabetes is a life-long (chronic) disease. If you have type 2 diabetes, the insulin your body normally makes has trouble transmitting a signal to muscle and fat cells. Insulin is a hormone made by the pancreas to control blood sugar. When your body's insulin isn't able to signal correctly, the sugar from food stays in the blood and the sugar (glucose) level can get too high. Most people with type 2 diabetes are overweight when they're diagnosed. The changes in the way the body handles blood sugar that lead to type 2 diabetes usually happen slowly. Everyone with diabetes should receive proper education and support about the best ways to manage their diabetes. Ask your health care provider about seeing a certified diabetes care and education specialist (often called a diabetes educator). Symptoms of Type 2 DiabetesYou may not have any symptoms. If you do have symptoms, they may include:
Take Control of Your DiabetesYou should have good control of your blood sugar. If your blood sugar is not controlled, serious problems called complications can happen to your body. Some complications can happen immediately and some after many years. Learn the basic steps for managing diabetes to stay as healthy as possible. Doing so will help keep the chance of having complications of diabetes as low as possible. Steps include:
Be sure to take any medicine or insulin as instructed. Your provider will also help you by ordering blood tests and other tests. These help make sure your blood sugar and cholesterol levels are each in a healthy range. Also, follow your provider's instructions about keeping your blood pressure in a healthy range. Your provider will likely ask you to visit other providers to help you control your diabetes. These providers include a:
Eat Healthy Foods and Manage Your WeightFoods with sugar or carbohydrates can raise your blood sugar too high. Alcohol and other drinks with sugar can also raise your blood sugar. A nurse or dietitian can teach you about good food choices. Make sure you know how to have a balanced meal with protein and fiber. Eat healthy, fresh foods as much as possible. Don't eat too much food at one sitting. This helps keep your blood sugar in a good range. Managing your weight and keeping a well-balanced diet are important. Some people with type 2 diabetes can stop taking medicines after losing weight (even though they still have diabetes). Your provider can let you know a good weight range for you. Weight-loss surgery may be an option if you are obese and your diabetes is not under control. Your provider can tell you more about this. ExerciseRegular exercise is good for people with diabetes. It lowers blood sugar. Exercise also:
It helps burn extra fat so that you can keep your weight down. Exercise can even help you handle stress and improves your mood. Try walking, jogging, or biking for 30 to 60 minutes every day. Pick an activity that you enjoy and you are more likely to stick with. Bring food or juice with you in case your blood sugar gets too low. Drink extra water. Try to avoid sitting for more than 30 minutes at any one time. Wear a diabetes ID bracelet. In case of an emergency, people know you have diabetes and can help you get the right medical attention. Always check with your provider before beginning an exercise program. Your provider can help you choose an exercise program that is safe for you. Check Your Blood SugarYou may be asked to check your blood sugar at home. This will tell you and your provider how well your diet, exercise, and medicines are working. A device called a glucose meter can provide a blood sugar reading from just a drop of blood. Your provider, nurse, or diabetes educator will help set up a home testing schedule for you. They will help you set your blood sugar goals.
The most important reasons to check your blood sugar are to:
You May Need MedicinesIf diet and exercise are not enough, you may need to take medicine. It will help keep your blood sugar in a healthy range. There are many diabetes medicines that work in different ways to help control your blood sugar. Many people with type 2 diabetes need to take more than one medicine to control their blood sugar. You may take medicines by mouth or as a shot (injection). Certain diabetes medicines may not be safe if you are pregnant. So, talk to your provider about your medicines if you're thinking of becoming pregnant. If some medicines don't help you control your blood sugar, you may need to take insulin. Most often, insulin must be injected under the skin. You'll receive special training to learn how to give yourself injections. Most people find that insulin injections are easier than they thought. Learn to Prevent Long-term Problems of DiabetesPeople with diabetes have a high chance of getting high blood pressure and high cholesterol. You may be asked to take medicine to prevent or treat these conditions. Medicines may include:
Do not smoke or use e-cigarettes. Smoking makes diabetes worse. If you do smoke, work with your provider to find a way to quit. Diabetes can cause foot problems. You may get sores or infections. To keep your feet healthy:
See Your Doctor RegularlyIf you have diabetes, you should see your provider every 3 months, or as often as instructed. At these visits, your provider may:
Your provider will also order blood and urine tests to make sure your:
Talk to your provider about any vaccines you may need, such as those for flu, COVID-19, hepatitis B, and pneumococcal infection (pneumonia). Visit the dentist every 6 months. Also, see your eye doctor once a year, or as often as instructed. ReferencesAmerican Diabetes Association Professional Practice Committee. 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes-2024 [published correction appears in Diabetes Care. 2024 Feb 05]. Diabetes Care. 2024;47(Suppl 1):S77-S110. PMID: 38078584 pubmed.ncbi.nlm.nih.gov/38078584/. American Diabetes Association Professional Practice Committee. 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S111-S125. PMID: 38078586 pubmed.ncbi.nlm.nih.gov/38078586/. American Diabetes Association Professional Practice Committee. 12. Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S231-S243. PMID: 38078577 pubmed.ncbi.nlm.nih.gov/38078577/. Brownlee M, Aiello LP, Sun JK, et al. Complications of diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 37. Riddle MC, Ahmann AJ. Therapeutics of type 2 diabetes. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 35. | ||
| ||
Review Date: 2/28/2024 Reviewed By: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


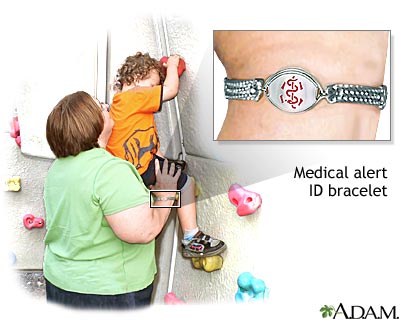 Medical alert brac...
Medical alert brac...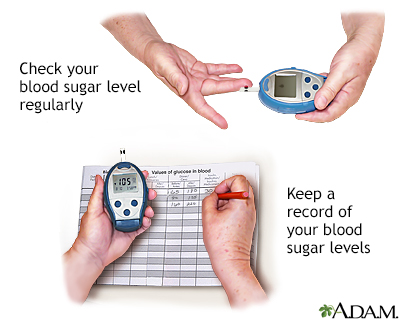 Manage your blood ...
Manage your blood ...
