Pregnancy SmartSiteTM
Shigella gastroenteritis; Shigella enteritis; Enteritis - shigella; Gastroenteritis - shigella; Traveler's diarrhea - shigellosis DefinitionShigellosis is a bacterial infection of the lining of the intestines. It is caused by a group of bacteria called Shigella. CausesThere are several types of Shigella bacteria, including:
People infected with the bacteria release it into their stool. They can spread the bacteria to water or food, or directly to another person. Getting just a little bit of the Shigella bacteria into your mouth is enough to cause infection. Outbreaks of shigellosis are linked to poor sanitation, contaminated food and water, and crowded living conditions. Shigellosis is common among travelers in developing countries and workers or residents in refugee camps. In the United States, the condition is most commonly seen in daycare centers and places where groups of people live, such as nursing homes. SymptomsSymptoms often develop about 1 to 7 days (average 3 days) after coming into contact with the bacteria. Symptoms include:
Exams and TestsIf you have symptoms of shigellosis, your health care provider will check for:
TreatmentThe goal of treatment is to replace fluids and electrolytes (salt and minerals) that are lost in diarrhea and stop the infection with antibiotics. Medicines that stop diarrhea are generally not given because they can cause the infection to take longer to go away. Self-care measures to avoid dehydration include drinking electrolyte solutions to replace the fluids lost by diarrhea. Several types of electrolyte solutions are available over-the-counter (without a prescription). Antibiotics can help shorten the length of the illness. These medicines also help prevent the illness from spreading to others in group living or daycare settings. They may also be prescribed for people with severe symptoms. If you have diarrhea and cannot drink fluids by mouth because of severe nausea, you may need medical care and intravenous (IV) fluids. This is more common in small children who have shigellosis. People who take diuretics ("water pills") may need to stop taking these medicines if they have acute Shigella enteritis. Never stop taking any medicine without first talking to your provider. Outlook (Prognosis)The infection can be mild and goes away on its own. Most people, except malnourished children and those with weakened immune systems, typically recover fully. Possible ComplicationsComplications may include:
About 1 in 10 children (under age 15) with severe Shigella enteritis develop nervous system problems. These may include febrile seizures (also called a "fever fit") when body temperature rises quickly and the child has seizures. A brain disease (encephalopathy) with headache, lethargy, confusion, and stiff neck can also develop. When to Contact a Medical ProfessionalContact your provider if diarrhea does not improve, if there is blood in the stool, or if there are signs of dehydration. Go to the emergency room if these symptoms occur in a person with shigellosis:
These symptoms are most common in children. PreventionPrevention includes properly handling, storing, and preparing food, and good personal hygiene. Handwashing is the most effective way to prevent shigellosis. Avoid food and water that may be contaminated. ReferencesFleckenstein JM. Approach to the patient with suspected enteric infection. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 262. Kotloff KL. Acute gastroenteritis in children. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 387. Lima AAM, Warren CA, Guerrant RL. Acute dysentery syndromes (diarrhea with fever). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 99. MacLennan CA. Shigellosis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 285. Melia JMP, Sears CL. Infectious enteritis and proctocolitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 110. | ||
| ||
Review Date: 3/16/2024 Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


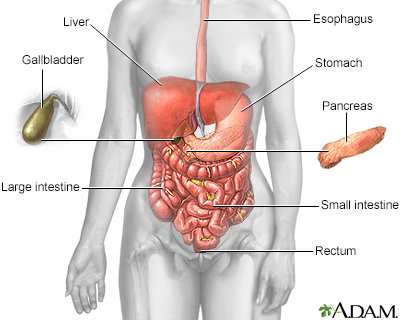 Digestive system
Digestive system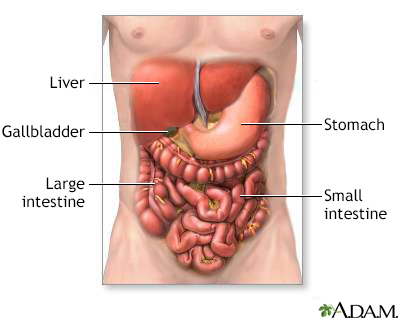 Digestive system o...
Digestive system o... Bacteria
Bacteria
