Intestinal polyps; Polyps - colorectal; Adenomatous polyps; Hyperplastic polyps; Villous adenomas; Serrated polyp; Serrated adenoma; Precancerous polyps; Colon cancer - polyps; Bleeding - colorectal polyps DefinitionA colorectal polyp is a growth on the lining of the colon or rectum. CausesPolyps of the colon and rectum are most often benign. This means they are not a cancer. You may have one or many polyps. They become more common with age. There are many types of polyps. Adenomatous polyps are a common type. They are gland-like growths that develop on the mucous membrane that lines the large intestine. They are also called adenomas and are most often one of the following:
When adenomas become cancerous, they are known as adenocarcinomas. Adenocarcinomas are cancers that originate in glandular tissue cells. Adenocarcinoma is the most common type of colorectal cancer. Other types of polyps are:
Polyps that are 1 centimeter (cm) or larger have a higher cancer risk than polyps smaller than 1 cm. Risk factors for these larger polyps include:
A small number of people with polyps may also be linked to some inherited disorders, including:
SymptomsPolyps usually do not have symptoms. When present, symptoms may include:
Exams and TestsYour health care provider will perform a physical exam. A large polyp in the rectum may be felt during a rectal exam. Most polyps are found with the following tests:
TreatmentColorectal polyps should be removed because some can develop into cancer. In most cases, the polyps may be removed during a colonoscopy. For people with adenomatous polyps, new polyps can appear in the future. You should have a repeat colonoscopy, usually 1 to 10 years later, depending on:
In rare cases, when polyps are very likely to turn into cancer or too large to remove during colonoscopy, the provider will recommend a partial colectomy. This is surgery to remove part of the colon that has the polyps. Outlook (Prognosis)The outlook is excellent if the polyps are removed. Polyps that are not removed can develop into cancer over time. When to Contact a Medical ProfessionalContact your provider if you have:
PreventionTo reduce your risk of developing polyps:
Your provider can order a colonoscopy or other screening tests:
Taking aspirin, naproxen, ibuprofen, or similar medicines may help reduce the risk for new polyps. Be aware that these medicines can have serious side effects if taken for a long time. Side effects include bleeding in the stomach or colon and heart disease. Talk with your provider before taking these medicines for this purpose. ReferencesCenters for Disease Control and Prevention. Colorectal cancer. Reducing risk for colorectal cancer. www.cdc.gov/colorectal-cancer/prevention/. Updated June 12, 2024. Accessed May 15, 2025. Chu E. Neoplasms of the small and large intestine. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 179. Garber JJ, Chung DC. Colonic polyps and polyposis syndromes. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 126. National Cancer Institute website. Colorectal cancer prevention (PDQ) - health professional version. www.cancer.gov/types/colorectal/hp/colorectal-prevention-pdq. Updated April 11, 2025. Accessed May 15, 2025. National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology (NCCN guidelines): colorectal cancer screening. Version 1.2024 - February 27, 2024. www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf. Updated February 27, 2024. Accessed May 15, 2025. Patel SG, May FP, Anderson JC, et al. Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2022;95(1):1-15. PMID: 34794803 pubmed.ncbi.nlm.nih.gov/34794803/. Qaseem A, Harrod CS, Crandall CJ, et al. Screening for colorectal cancer in asymptomatic average-risk adults: a guidance statement from the American College of Physicians (Version 2). Ann Intern Med. 2023;176(8):1092-1100. PMID: 37523709 pubmed.ncbi.nlm.nih.gov/37523709/. US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(19):1965-1977. PMID: 34003218 pubmed.ncbi.nlm.nih.gov/34003218/. | ||
| ||
Review Date: 4/21/2025 Reviewed By: Todd Eisner, MD, Private practice specializing in Gastroenterology in Boca Raton and Delray Beach, Florida at Gastroenterology Consultants of Boca Raton. Affiliate Assistant Professor, Florida Atlantic University School of Medicine. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||

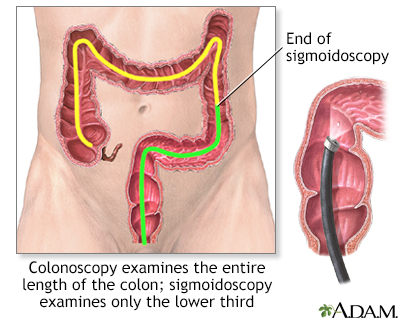 Colonoscopy
Colonoscopy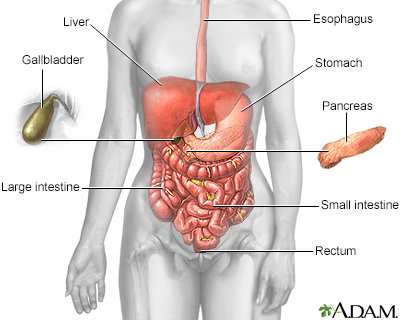 Digestive system
Digestive system
