Antibiotic-associated colitis; Colitis - pseudomembranous; Necrotizing colitis; C difficile - pseudomembranous; C diff DefinitionPseudomembranous colitis refers to swelling or inflammation of the large intestine (colon) due to an overgrowth of Clostridioides difficile (C difficile) bacteria. This infection is a common cause of diarrhea after antibiotic use. Not all cases of diarrhea associated with antibiotic use are due to C difficile or will progress to pseudomembranous colitis. CausesThe C difficile bacteria normally lives in the intestine. However, too much of these bacteria may grow when you take antibiotic medicines. The bacteria give off a strong toxin that causes inflammation and bleeding in the lining of the colon. Any antibiotic can cause this condition. The medicines responsible for the problem most of the time are ampicillin, clindamycin, fluoroquinolones, and cephalosporins. Health care providers in the hospital may pass this bacteria from one patient to another. Pseudomembranous colitis is uncommon in children, and rare in infants. It is most often seen in people who are in the hospital. However, it is becoming more common in people who take antibiotics and are not in a hospital. Risk factors include:
SymptomsSymptoms include:
Exams and TestsThe following tests may be done:
TreatmentThe antibiotic or other medicine causing the condition should be stopped. Fidaxomicin and vancomycin are most often used to treat the problem. Metronidazole is also effective, but it is no longer a first line choice in the US. Electrolyte solutions or fluids given through a vein may be needed to treat dehydration due to diarrhea. In rare cases, surgery is needed to treat infections that get worse or do not respond to antibiotics. Long term antibiotics may be needed if the C difficile infection returns. A treatment called fecal microbiota transplant ("stool transplant") has also been effective for infections that come back. Your provider may also suggest that you take probiotics if the infection returns. An antibody treatment may be needed in patients with very high risk of recurrent C difficile to lessen the risk of recurrence. Outlook (Prognosis)The outlook is good in most cases, if there are no complications. However, up to 1 in 5 infections may return and need more treatment. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalContact your provider if you have the following symptoms:
PreventionPeople who have had pseudomembranous colitis should tell their providers before taking antibiotics again. It is also very important to wash hands well to prevent passing the germ to other people. Alcohol sanitizers do not always work on C difficile. ReferencesGerding DN, Young VB. Donskey CJ. Clostridiodes difficile (formerly Clostridium difficle) infection. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 243. Johnson S, Lavergne V, Skinner AM, et al. Clinical practice guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 focused update guidelines on management of clostridioides difficile infection in adults. Clin Infect Dis. 2021; 73(5):e1029-e1044. PMID: 34164674 pubmed.ncbi.nlm.nih.gov/34164674/. Kelly CP, Khanna S. Antibiotic-associated diarrhea and clostridioides difficile infection. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 112. Wilcox MH, Dubberke ER. Clostridial and Clostridioides infections. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 271. | ||
| ||
Review Date: 5/14/2024 Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||

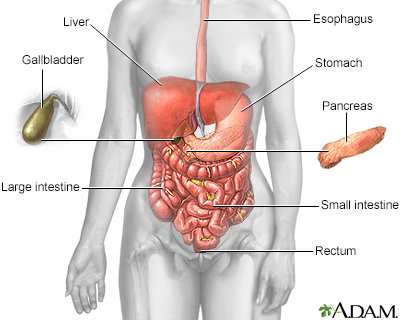 Digestive system
Digestive system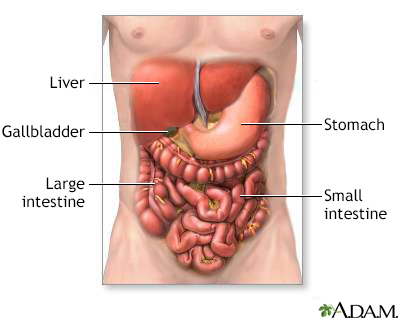 Digestive system o...
Digestive system o...
