Pregnancy SmartSiteTM
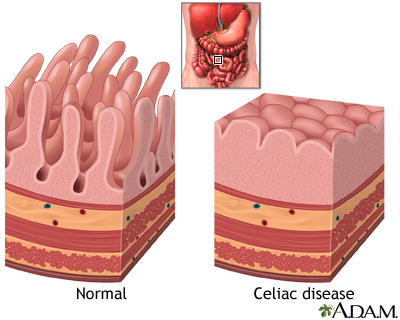
Sprue; Nontropical sprue; Gluten intolerance; Gluten-sensitive enteropathy; Celiac sprue DefinitionCeliac disease is an autoimmune condition that damages the lining of the small intestine. This damage comes from a reaction to eating gluten. This is a substance that is found in wheat, rye, barley, and possibly oats. It is also found in food made from these ingredients. The damaged intestine is not able to fully absorb nutrients from food. CausesThe exact cause of celiac disease is not known. The lining of the intestines have small areas called villi which project outward into the opening of the intestine. These structures help absorb nutrients. When people with celiac disease eat foods with gluten, their immune system reacts by damaging the villi. Because of the damage, the villi are unable to properly absorb iron, vitamins, and other nutrients. This may cause a number of symptoms and other health problems. The disease can develop at any point in life, from infancy to late adulthood. People who have a family member with celiac disease are at greater risk of developing the disease. The disorder is most common in Europeans. People with celiac disease are more likely to have:
SymptomsThe symptoms of celiac disease can be different from person to person. This can make diagnosis difficult. For example, one person may have constipation, a second may have diarrhea, and a third may have no problem with stools. Gastrointestinal symptoms include:
Other problems that can develop over time because the intestines do not absorb key nutrients include:
Children with celiac disease may have:
Exams and TestsThe following tests may be performed:
Blood tests can detect antibodies, called antitissue transglutaminase antibodies (tTGA) or anti-endomysial antibodies (EMA) which may help detect the condition. The health care provider will order these antibody tests if celiac disease is suspected. If the tests are positive, upper endoscopy is often performed to sample a piece of tissue (biopsy) from the first part of the small intestine (duodenum). The biopsy may show a flattening or loss of the villi in the parts of the intestine affected in the duodenum. Genetic testing of the blood can also be done to help detect who may be at risk for celiac disease. Those who test negative for the common genetic variant are unlikely to have celiac disease. A follow-up biopsy or blood test may be ordered several months after the diagnosis and treatment. These tests assess how well treatment is working. Normal results mean that you have responded to treatment. This confirms the diagnosis. However, this does not mean that the disease has been cured. TreatmentCeliac disease cannot be cured. Your symptoms will go away and the villi in the intestines will heal if you follow a lifelong gluten-free diet. Do not eat foods, drink beverages, or take medicines that contain wheat, barley, rye, and possibly oats. You must read food and drug labels carefully to look for ingredients that may include these grains. It may be hard to stick to a gluten-free diet because wheat and barley grains are common in the American diet. Over time, most people are able to adapt and get better. You should NOT begin the gluten-free diet before you are diagnosed. Starting the diet will affect testing for the disease. In most cases, following a well-balanced, gluten-free diet is the only treatment you need to stay well. Your provider may need to prescribe vitamin and mineral supplements. Sometimes, short-term use of corticosteroids (such as prednisone) may be needed if celiac disease does not respond to treatment. When you are diagnosed, get help from a registered dietitian who specializes in celiac disease and the gluten-free diet. A support group may also help you cope with the disease and diet. Support GroupsYou can ease the stress of illness by joining a support group. More information and support for people with celiac disease and their families can be found at the National Celiac Association. Outlook (Prognosis)Following a gluten-free diet heals the damage to the intestines and prevents further damage. This healing most often occurs within 3 to 6 months in children. Recovery may take 2 to 3 years in adults. Rarely, long-term damage will be done to the lining of the intestines before the diagnosis is made. Some problems caused by celiac disease may not improve, such as a short height and damage to the teeth. Possible ComplicationsYou must carefully continue to follow the gluten-free diet. When untreated, the disease can cause fatal complications. Delaying diagnosis or not following the diet puts you at risk for related conditions such as:
When to Contact a Medical ProfessionalContact your provider if you have symptoms of celiac disease. PreventionBecause the exact cause is not known, there is no way to prevent the development of celiac disease. However, you should be aware of the risk factors such as family history. This may increase your chances of early diagnosis and treatment. ReferencesLebwohl B, Green PHR. Celiac disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 107. Lin JC, Benz EJ Jr. Approach to anemia in the adult and child. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 35. Rubio-Tapia A, Hill ID, Semrad C, et al. American College of Gastroenterology guidelines update: diagnosis and management of celiac disease. Am J Gastroenterol. 2023;118(1):59-76. PMID: 36602836 pubmed.ncbi.nlm.nih.gov/36602836/. Schiller LR. Malabsorption. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2024. Philadelphia, PA: Elsevier; 2024:273-279. Semrad CE. Approach to the patient with diarrhea and malabsorption. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 126. | ||
| ||
Review Date: 3/31/2024 Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Celiac disease
Celiac disease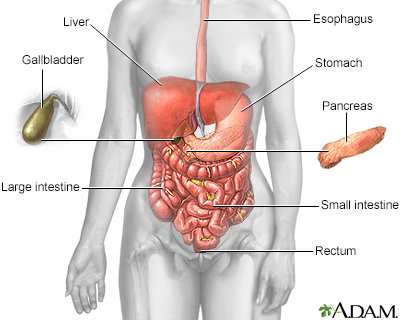 Digestive system
Digestive system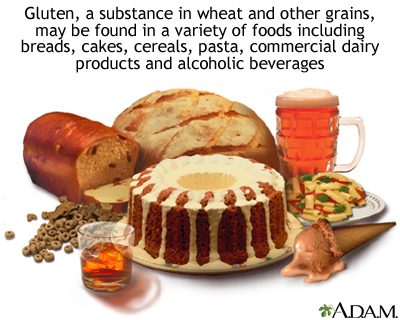 Celiac sprue - foo...
Celiac sprue - foo... Dermatitis - herpe...
Dermatitis - herpe... Dermatitis - herpe...
Dermatitis - herpe...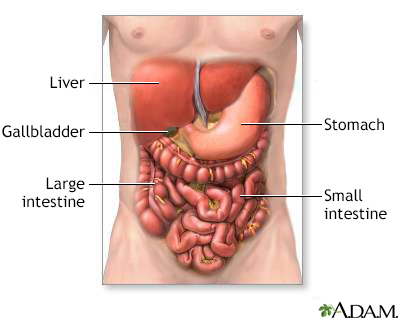 Digestive system o...
Digestive system o...
