  |
Blood Group (Rh) Incompatibility
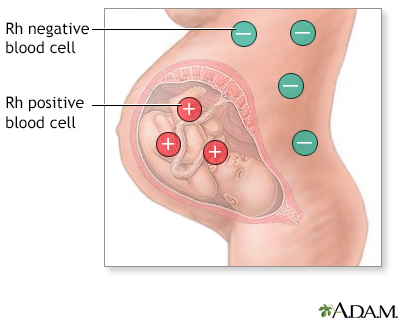
Rh incompatibility occurs when the mother's blood type is Rh negative and her fetus's blood type is Rh positive. An alternative name is Rh disease. Rh is an abbreviation for Rhesus.
What Is It?
Everyone is born with a certain blood type that is either Rh positive or Rh negative. Rh-positive blood is more common than Rh-negative blood. About 85% of Caucasians are Rh positive, while the percentage is even higher for African-Americans, Asians, and American Indians. If you are Rh positive, or if both you and the baby's father are Rh negative, there is no reason to worry about Rh incompatibility. However, if you are Rh negative and the baby's father is Rh positive, then your baby may inherit the father's blood type, creating incompatibility between you and the fetus.
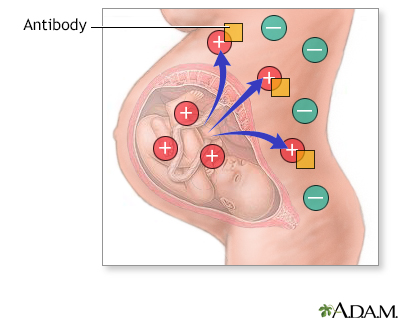
With Rh incompatibility, if some of the fetal blood gets into your bloodstream, your body will produce antibodies. These antibodies could pass back through the placenta and harm the developing baby's red blood cells, causing very mild to very serious anemia in the fetus. Your first baby is usually safe, because fetal and maternal blood usually do not mix until delivery. If your second baby is also Rh positive, there’s a risk that your antibodies will attack her blood cells and cause problems.

How Do I Know I Have It?
There aren't any physical symptoms that would allow you to detect on your own if you are Rh incompatible with your baby. If you are pregnant, it is standard procedure for your health care provider to order a blood test that will determine whether you are Rh positive or Rh negative. If the blood test indicates that you have developed Rh antibodies, your blood will be monitored regularly to assess the level of antibodies it contains. If the levels are high, an amniocentesis is performed to determine the degree of anemia in the fetus.
How Can I Treat It?
During prenatal care, a doctor will usually take measures that prevent an Rh-negative mother from developing antibodies in response to the Rh-positive blood of the fetus. Your baby may be monitored with ultrasounds to look for signs of anemia.
If antibodies are present and anemia is detected in the fetus, a blood transfusion is performed to replace the fetus's blood supply with Rh-negative blood, which will not be damaged by the antibodies your body has created. The transfusion is administered through the umbilical cord while the fetus is still in the uterus, beginning at 18 weeks of pregnancy or beyond. This procedure can be somewhat risky, so some doctors prefer to induce an early labor. The blood transfusion is then administered after the baby is born.
How Can I Prevent It?
Rh disease is rare today, because mothers who are Rh negative receive intramuscular injections with a drug called Rhogam. Rhogam removes Rh positive fetal cells from the mother’s bloodstream before her body recognizes them and begins making antibodies. All mothers who are Rh negative receive a shot of Rhogam around 28 weeks. You may get an extra shot if you have bleeding early in pregnancy, or if you have a procedure such as an amniocentesis that might cause fetal blood cells to be mixed into your circulation.
If your baby is born Rh positive, another dose is administered within 72 hours after delivery. This will prevent your body from creating any future antibodies that could cause harm during a subsequent pregnancy.
Frequently Asked Questions
Q: If my baby is born Rh negative, but I have received the Rh-immune globulin vaccine, will he be harmed?
A: No. There is no risk from the vaccine to either you or your baby. It's always best to be cautious and administer it, even if your baby turns out to be Rh negative instead of Rh positive.
Q: Why are some people born with Rh-positive blood while others are born with Rh-negative blood?
A: Blood groups are determined by the specific amount of protein molecules that appear on the surface of your blood cells. The Rh factor is one of these blood groups. Only a small portion of the population is Rh negative.
Q: What are my chances of getting Rh disease during my first pregnancy?
A: There is a slight possibility of the fetal blood entering your bloodstream through the placenta or during an amniocentesis in a first-time pregnancy. That’s why Rhogam is given if you have any procedures that could stir up fetal and maternal blood. Usually, Rh disease only occurs during second or subsequent pregnancies.
Reviewed By: Irina Burd, MD, PhD, Maternal Fetal Medicine, Johns Hopkins University, Baltimore, MD. Review provided by VeriMed Healthcare Network.
© 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
