Pregnancy SmartSiteTM
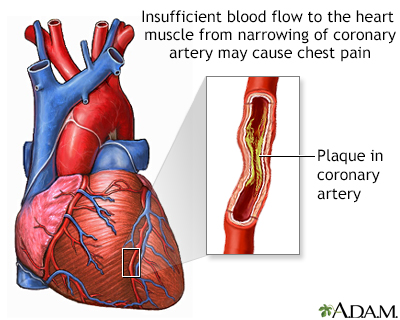
Accelerating angina; New-onset angina; Angina - unstable; Progressive angina; CAD - unstable angina; Coronary artery disease - unstable angina; Heart disease - unstable angina; Chest pain - unstable angina DefinitionUnstable angina is a condition in which your heart doesn't get enough blood flow and oxygen. It may lead to a heart attack. Angina is a type of chest discomfort due to poor blood flow through the blood vessels in the heart called the coronary arteries. CausesCoronary artery disease due to atherosclerosis is the most common cause of unstable angina. Atherosclerosis is the buildup of fatty material, called plaque, along the walls of the arteries. This causes arteries to become narrowed and less flexible. The narrowing can reduce blood flow to the heart, causing chest pain (angina). Unstable angina is a special subset of angina and is defined below. People with unstable angina are at higher risk of having a heart attack. Less common causes of angina are:
Risk factors for coronary artery disease include:
SymptomsSymptoms of angina may include:
With stable angina, the chest pain or other symptoms only occur with a certain amount of activity or stress. The pain does not occur more often or get worse over time. Unstable angina is chest pain that is sudden and often gets worse over a short period of time. You may be developing unstable angina if your chest pain:
Unstable angina is a warning sign that a heart attack may happen soon and needs to be treated right away. Contact your health care provider if you have any type of chest pain. Exams and TestsYour provider will do a physical exam and check your blood pressure. Your provider may hear abnormal sounds, such as a heart murmur or irregular heartbeat, when listening to your chest with a stethoscope. Tests for angina include:
TreatmentYou may need to check into the hospital to get some rest, have more tests, and prevent complications. Certain blood thinners (antiplatelet medicines) are used to treat and prevent unstable angina. You will receive these medicines as soon as possible if you can take them safely. Medicines include aspirin and the prescription medicine clopidogrel or something similar (ticagrelor, prasugrel). These medicines may be able to reduce the chance of a heart attack or the severity of a heart attack that occurs. During an unstable angina event:
A procedure called angioplasty and stenting can often be done to open a blocked or narrowed artery.
Heart bypass surgery may be done for some people. The decision to have this surgery depends on:
Outlook (Prognosis)Unstable angina is a sign of more severe heart disease. How well you do depends on many different things, including:
Abnormal heart rhythms and heart attacks can cause sudden death. Possible ComplicationsUnstable angina may lead to:
When to Contact a Medical ProfessionalSeek medical attention right away if you have new, unexplained chest pain or pressure. If you have had angina before, contact your provider. Call 911 or the local emergency number if your angina pain:
Contact your provider right away if:
If you think you are having a heart attack, get medical treatment right away. PreventionSome studies have shown that making a few lifestyle changes can prevent blockages from getting worse and may actually improve them. Lifestyle changes can also help prevent some angina attacks. Your provider may tell you to:
Your provider will also recommend that you keep other health conditions such as high blood pressure, diabetes, and high cholesterol levels under control. If you have one or more risk factors for heart disease, talk to your provider about taking aspirin or other medicines to help prevent a heart attack. Aspirin therapy (75 to 325 mg a day) or medicines such as clopidogrel, ticagrelor or prasugrel may help prevent heart attacks in some people. Aspirin and other blood-thinning therapies are recommended if the benefit is likely to outweigh the risk of side effects. ReferencesBonaca MP, Sabatine MS. Approach to the patient with chest pain. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 35. Giugliano RP, Braunwald E. Non-ST elevation acute coronary syndromes. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 39. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368-e454. PMID: 34709879 pubmed.ncbi.nlm.nih.gov/34709879/. Lange RA, Mukherjee D. Acute coronary syndrome: unstable angina and non-ST elevation myocardial infarction. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 57. Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. Published online February 27, 2025. PMID: 40014670 pubmed.ncbi.nlm.nih.gov/40014670/. Writing Committee Members; Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):e187-e285. PMID: 34756653 pubmed.ncbi.nlm.nih.gov/34756653/. | ||
| ||
Review Date: 1/1/2025 Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Angina
Angina
