Pregnancy SmartSiteTM
Cardiomyopathy - peripartum; Cardiomyopathy - pregnancy DefinitionPeripartum cardiomyopathy is a rare disorder in which a pregnant woman's heart becomes weakened and enlarged. It develops during the last month of pregnancy, or within 5 months after the baby is born. CausesCardiomyopathy occurs when there is damage to the heart muscle. As a result, the heart muscle becomes weak and does not pump well. This affects the lungs, liver, and other body systems. Peripartum cardiomyopathy is a form of dilated cardiomyopathy in which no other cause of heart weakening can be found. It may occur in pregnant women of any age, but it is most common after age 30. Risk factors for the condition include:
SymptomsSymptoms may include:
Exams and TestsDuring a physical exam, the health care provider will look for signs of fluid in the lungs by touching and tapping with the fingers. A stethoscope will be used to listen for lung crackles, a rapid heart rate, or abnormal heart sounds. The liver may be enlarged and neck veins may be swollen. Blood pressure may be low or may drop when standing up. Heart enlargement, congestion of the lungs or the veins in the lungs, decreased cardiac output, decreased movement or functioning of the heart, or heart failure may show up on: A heart biopsy may help determine if the underlying cause of cardiomyopathy is a heart muscle infection (myocarditis). However, this procedure is not done very often. TreatmentA woman may need to stay in the hospital until acute symptoms subside. Because it is very often possible to restore heart function, and the women who have this condition are often young and otherwise healthy, care is often aggressive. When severe symptoms occur, this may include extreme steps such as:
For most women, however, treatment mainly focuses on relieving the symptoms. Some symptoms go away on their own without treatment. Medicines that are often used include:
A low-salt diet may be recommended. Fluid may be restricted in some cases. Activities, including nursing the baby, may be limited when symptoms develop. Daily weighing may be recommended. A weight gain of 3 to 4 pounds (1.5 to 2 kilograms) or more over 1 or 2 days may be a sign of fluid buildup. Women who smoke and drink alcohol will be advised to stop, since these habits may make the symptoms worse. Outlook (Prognosis)There are several possible outcomes in peripartum cardiomyopathy. Some women remain stable for long periods, while others get worse slowly. Others get worse very quickly and may be candidates for a heart transplant. About 4% of people will require heart transplantation and 9% may die suddenly or die from complications of the procedure. The outlook is good when a woman's heart returns to normal after the baby is born. If the heart remains abnormal, future pregnancies may result in heart failure. It is not known how to predict who will recover and who will develop severe heart failure. Up to about one half of women will recover completely. Women who develop peripartum cardiomyopathy are at high risk of developing the same problem with future pregnancies. The rate of recurrence is about 30%. Therefore, women who have had this condition should discuss birth control methods with their provider. Possible ComplicationsComplications include:
When to Contact a Medical ProfessionalContact your provider if you are currently pregnant or have recently delivered a baby and think you may have signs of cardiomyopathy. Get medical help right away if you develop chest pain, palpitations, faintness, or other new or unexplained symptoms. PreventionEat a well-balanced diet and get regular exercise to help keep your heart strong. Avoid cigarettes and alcohol. Your provider may advise you to avoid getting pregnant again if you have had heart failure during a previous pregnancy. ReferencesBlanchard DG, Daniels LB, Alshawabkeh L. Cardiac diseases. In: Lockwood CJ, Copel JA, Dugoff L et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 52. Elliott PM, Olivotto I. Diseases of the myocardium and endocardium. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 47. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(17):1757-1780. PMID: 35379504 pubmed.ncbi.nlm.nih.gov/35379504/. Silversides CK, Siu SC. Pregnancy and heart disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 92. | ||
| ||
Review Date: 5/27/2024 Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 02/05/2025. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Heart - section th...
Heart - section th... Heart - front view
Heart - front view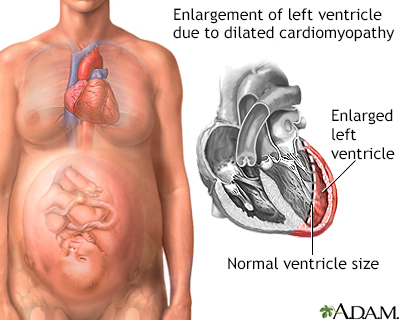 Peripartum cardiom...
Peripartum cardiom...
