Pregnancy SmartSiteTM
Tricuspid insufficiency; Heart valve - tricuspid regurgitation; Valvular disease - tricuspid regurgitation DefinitionBlood that flows between different chambers of your heart must pass through a heart valve. These valves open up enough so that blood can flow through. They then close, keeping blood from flowing backward. The tricuspid valve separates the right lower heart chamber (the right ventricle) from the right upper heart chamber (right atrium). Tricuspid regurgitation is a disorder in which this valve does not close tight enough. This problem causes blood to flow backward into the right atrium when the right ventricle contracts. CausesAn increase in size of the right ventricle is the most common cause of this condition. The right ventricle pumps blood to the lungs where it picks up oxygen. Any condition that puts extra strain on this chamber can cause it to enlarge. Examples include:
Tricuspid regurgitation may also be caused or worsened by infections, such as:
Less common causes of tricuspid regurgitation include:
SymptomsMild tricuspid regurgitation may not cause any symptoms. Symptoms of heart failure may occur, and can include:
Exams and TestsThe health care provider may find abnormalities when gently pressing with the hand (palpating) on your chest. The provider may also feel a pulse over your liver. The physical exam may show liver and spleen swelling. Listening to the heart with a stethoscope may reveal a murmur or other abnormal sounds. There may be signs of fluid buildup in the abdomen. An electrocardiogram (ECG) or echocardiogram may show enlargement of the right side of the heart. Doppler echocardiography or right-sided cardiac catheterization may be used to measure blood pressure inside the heart and lungs. Other tests, such as CT scan or MRI of the chest (heart), may reveal enlargement of the right side of the heart and other changes. TreatmentTreatment may not be needed if there are few or no symptoms. You may need to go to the hospital to diagnose and treat severe symptoms. Swelling and other symptoms of heart failure may be managed with medicines that help remove fluids from the body (diuretics). Some people may be able to have surgery to repair or replace the tricuspid valve. Surgery is most often done as part of another procedure. Catheter-based procedures for tricuspid valve disease are in development. Treatment of certain conditions may correct this disorder. These include:
Outlook (Prognosis)Surgical valve repair or replacement most often provides a cure in people who need an intervention. The outlook is poor for people who have symptomatic, severe tricuspid regurgitation that cannot be corrected. When to Contact a Medical ProfessionalContact your provider if you have symptoms of tricuspid regurgitation. PreventionPeople with abnormal or damaged heart valves are at risk for an infection called endocarditis. Anything that causes bacteria to get into your bloodstream may lead to this infection. Steps to avoid this problem include:
Prompt treatment of disorders that can cause valve or other heart diseases reduces your risk for tricuspid regurgitation. ReferencesCarabello BA, Kodali S. Valvular heart disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 60. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143(5):e35-e71. PMID: 33332149 pubmed.ncbi.nlm.nih.gov/33332149/. Pellikka PA, Nkomo VT. Tricuspid, pulmonic, and multivalvular disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 77. Rosengart TK, Aberle CM, Ryan C. Acquired heart disease: valvular. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 61. | ||
| ||
Review Date: 2/27/2024 Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


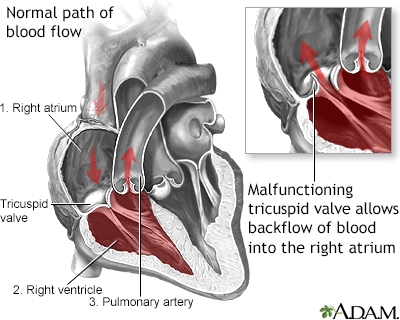 Tricuspid Regurgit...
Tricuspid Regurgit...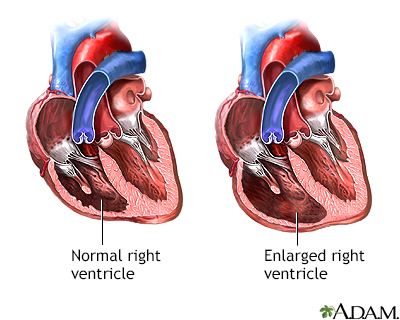 Tricuspid Regurgit...
Tricuspid Regurgit...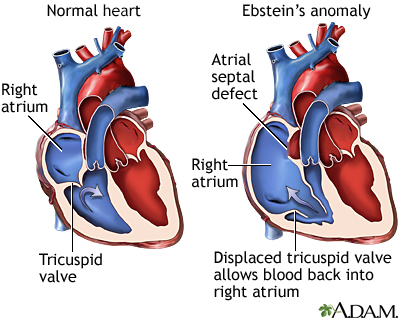 Ebstein's anomaly
Ebstein's anomaly
