Pregnancy SmartSiteTM
Bronchopneumonia; Community-acquired pneumonia; CAP DefinitionPneumonia is inflamed or swollen lung tissue due to infection with a germ. This article covers community-acquired pneumonia (CAP). This type of pneumonia is found in people who have not recently been in the hospital or another health care facility such as a nursing home or rehab facility. Pneumonia that affects people in or recently released from a health care facility, such as hospitals, is called hospital-acquired pneumonia (or health care-associated pneumonia). CausesPneumonia is a common illness that affects millions of people each year in the United States. Germs called bacteria, viruses, and fungi may cause pneumonia. In adults, bacteria are the most common cause of pneumonia. Ways you can get pneumonia include:
Pneumonia can be caused by many types of germs.
Risk factors that increase your chance of getting pneumonia include:
SymptomsThe most common symptoms of pneumonia are:
Other symptoms include:
Exams and TestsYour health care provider will listen for crackles or abnormal breath sounds when listening to your chest with a stethoscope. Tapping on your chest wall (percussion) helps your provider listen and feel for abnormal sounds in your chest. If pneumonia is suspected, your provider will likely order a chest x-ray. Other tests that may be ordered include:
TreatmentYour provider must first decide whether you need to be in the hospital. If you are treated in the hospital, you will receive:
If you are diagnosed with a bacterial form of pneumonia, it is important that you are started on antibiotics very soon after you are admitted. If you have viral pneumonia, you will not receive antibiotics. This is because antibiotics do not kill viruses. You may receive other medicines, such as antivirals, if you have the flu or other type of viral pneumonia. You are more likely to need to be admitted to the hospital if you:
Most people can be treated at home. If so, your provider may tell you to take medicines such as antibiotics. Antibiotics are usually prescribed for 3 to 5 days, although sometimes they may be used for 2 weeks or more. When taking antibiotics:
Breathing warm, moist (wet) air helps loosen the sticky mucus that may make you feel like you are choking. These things may help:
Drink plenty of liquids, as long as your provider says it is OK.
Get plenty of rest when you go home. If you have trouble sleeping at night, take naps during the day. Outlook (Prognosis)With treatment, most people improve rapidly and feel nearly back to normal within 2 weeks. Older adults or very sick people may need longer treatment. Those who may be more likely to have complicated pneumonia include:
In all of the above conditions, pneumonia can lead to serious illness or even death, if it is severe. In rare cases, more serious problems may develop, including:
After treatment, your provider may order another x-ray. This is to make sure your lungs are clear. But it may take many weeks for your x-ray to clear up. You will likely feel better before the x-ray clears up. When to Contact a Medical ProfessionalContact your provider if you have:
PreventionYou can help prevent pneumonia by following the measures below. Wash your hands often, especially:
Avoid coming into contact with people who are sick. Do not smoke. Tobacco damages your lung's ability to fight infection. Vaccines may help prevent some types of pneumonia. Be sure to get the following vaccines:
Vaccines are even more important for older adults and people with heart disease, diabetes, asthma, emphysema, HIV, cancer, people with organ transplants, or other long-term conditions. ReferencesBaden LR, Griffin MR, Klompas M. Overview of pneumonia. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 85. Daly JS, Ellison RT. Acute pneumonia. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 67. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. PMID: 31573350 pubmed.ncbi.nlm.nih.gov/31573350/. | ||
| ||
Review Date: 8/19/2024 Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


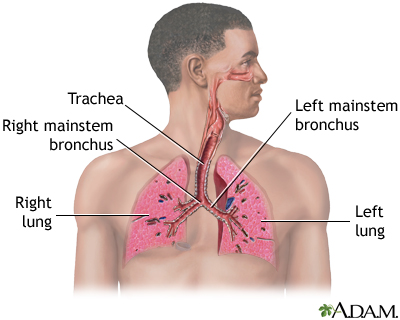 Respiratory system
Respiratory system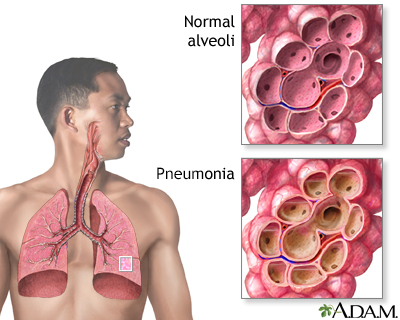 Pneumonia
Pneumonia White nail syndrom
White nail syndrom
