Pregnancy SmartSiteTM
Loss of bladder control - care at home; Uncontrollable urination - care at home; Stress incontinence - care at home; Bladder incontinence - care at home; Pelvic prolapse - care at home; Leakage of urine - care at home; Urinary leakage - care at home DescriptionYou have urinary incontinence. This means you are not able to prevent urine from leaking from your urethra. This is the tube that carries urine out of your body from your bladder. Urinary incontinence may occur because of aging, surgery, weight gain, neurologic disorders, or childbirth. There are many things you can do to help keep urinary incontinence from affecting your daily life. Skin CareYou may need to take special care of the skin around your urethra. These steps may help. Clean the area around your urethra right after urinating. This will help keep the skin from getting irritated. It will also prevent infection. Ask your health care provider about special skin cleaners for people who have urinary incontinence.
Use warm water and wash gently when bathing. Scrubbing too hard can hurt the skin. After bathing, use a moisturizer and a barrier cream.
Ask your provider about deodorizing tablets to help with odor. Clean your mattress if it becomes wet.
You can also use water-resistant sheets to keep urine from soaking into your mattress. DietEat healthy foods and exercise regularly. Try to lose weight if you are overweight. Being too heavy will weaken the muscles that help you stop urinating. Drink plenty of water:
Do not drink anything 2 to 4 hours before going to bed. Empty your bladder before going to bed to help prevent urine leakage during the night. Avoid foods and beverages that can make urine leakage worse. These include:
Get more fiber in your diet, or take fiber supplements to prevent constipation. Follow these steps when you exercise:
Controlling the Need to UrinateSome activities may increase leakage for some people. Things to avoid include:
Ask your provider about things you can do to ignore urges to pass urine. After a few weeks, you should leak urine less often. Train your bladder to wait a longer time between trips to the toilet.
Urinate at set times, even if you do not feel the urge. Schedule yourself to urinate every 2 to 4 hours. Empty your bladder all the way. After you go once, go again a few minutes later. Even though you are training your bladder to hold in urine for longer periods of time, you should still empty your bladder more often during times when you might leak. Set aside specific times to train your bladder. Urinate often enough at other times when you are not actively trying to train your bladder to help prevent incontinence. Ask your provider about medicines that may help. Surgery may be an option for you. Ask your provider if you would be a candidate. Pelvic Floor Muscle StrengtheningYour provider may recommend Kegel exercises. These are exercises in which you tighten the muscles that you use to stop urine flow. You may more easily learn how to do these exercises correctly using biofeedback. Your provider will help you learn how to tighten your muscles while you are being monitored with a computer. It may help to have formal pelvic floor physical therapy. The therapist can give you guidance on how to do the exercises to get the most benefit. ReferencesNewman DK, Burgio KL. Conservative management of urinary incontinence: behavioral and pelvic floor therapy and urethral and pelvic devices. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 121. Patton S, Bassaly RM. Urinary incontinence. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2024. Philadelphia, PA: Elsevier; 2024:1201-1203. Resnick NM, DuBeau CE. Urinary incontinence. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 115. | ||
| ||
Review Date: 9/2/2024 Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


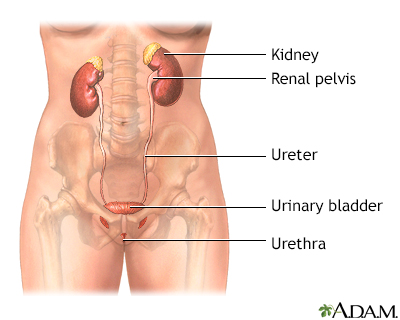 Female urinary tra...
Female urinary tra... Male urinary tract
Male urinary tract
