| Rheumatoid arthritis |
Rheumatoid arthritis is a chronic (long-term) inflammatory disease that primarily affects the joints and surrounding tissues, but can also affect other organ systems.
The cause of rheumatoid arthritis (RA) is unknown. However, RA involves an attack on the body by its own immune cells. Different cases may have different causes. Infectious, genetic, and hormonal factors may play a role.
The disease can occur at any age, but it begins most often between the ages of 25 and 55. The disease is more common in older people. Women are affected more often than men. About 1 to 2% of the total population is affected. The course and the severity of the illness can vary considerably.
The disease usually begins gradually, with fatigue, morning stiffness, diffuse muscle aches, loss of appetite, and weakness. Eventually, joint pain appears, with warmth, swelling, tenderness, and stiffness of the joint after inactivity.
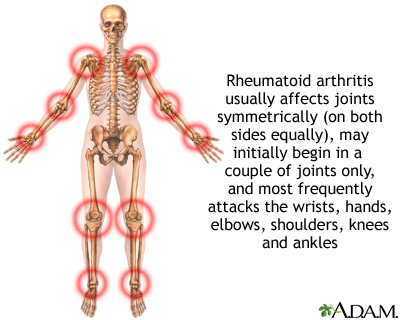
RA usually affects joints on both sides of the body equally. Wrists, fingers, knees, feet, and ankles are the most commonly affected.
When the synovium (the lining of the joint) becomes inflamed, it secretes more fluid and the joint becomes swollen. Later, the cartilage becomes rough and pitted. The underlying bone is eventually affected. Joint destruction may begin, often within 1 to 2 years after the appearance of the disease.
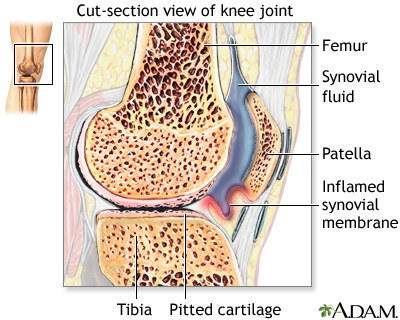
Deformities result from cartilage destruction, bone erosions, and tendon inflammation and rupture. A life-threatening joint complication can occur when the cervical spine becomes unstable as a result of RA.

Other features
Other features of the disease that do not involve the joints may occur. Rheumatoid nodules are painless, hard, round or oval masses that appear under the skin, usually on pressure points, such as the elbow or Achilles tendon.
On occasion, nodules appear in the eye where they sometimes cause inflammation. If they occur in the lungs, inflammation of the lining of the lung (pleurisy) may occur, causing shortness of breath and fluid accumulation in the lung.
Anemia may occur due to failure of the bone marrow to produce enough new red cells to make up for the lost ones. Iron supplements will not usually help. Other blood abnormalities can also be found, such as platelet counts that are either too high or too low.
Rheumatoid vasculitis (inflammation of the blood vessels) is a serious complication of RA and can be life-threatening. It can lead to skin ulcerations (and subsequent infections), bleeding stomach ulcers (which can lead to massive hemorrhage), and neuropathies (nerve problems causing pain, numbness or tingling).
Vasculitis may also affect the brain, nerves, and heart, causing strokes, sensory neuropathies (numbness and tingling), heart attacks, or heart failure.
Heart complications of RA commonly affect the outer lining of the heart. When inflamed, the condition is referred to as pericarditis. Inflammation of heart muscle, called myocarditis, can also develop. Both of these conditions can lead to congestive heart failure, characterized by shortness of breath and fluid accumulation in the lung.
Eye complications include inflammation of various parts of the eye. These must be screened for in RA patients.
Treatment
RA usually requires lifelong treatment, including various medications, physical therapy, education, and possibly surgery to relieve the symptoms of the disease. Early, aggressive treatment can delay joint destruction.
In addition to rest, strengthening exercises, and anti-inflammatory drugs, the current standard of care is to begin aggressive therapy with disease-modifying anti-rheumatic drugs (DMARDs), once the diagnosis is confirmed.
DMARDs, commonly used to initiate therapy, include methotrexate, hydroxychloroquine, and sulfasalazine. Minocycline may be as effective or more effective than hydroxychloroquine. Methotrexate is the most commonly used initial DMARD agent.
Increasingly, combination therapy is being used for added effectiveness. The idea of "triple therapy," using methotrexate, hydroxychloroquine, and sulfasalazine together, has been found to be more effective than any one of the drugs alone. Combining methotrexate with a variety of other individual drugs may add benefit as well.
In the last few years, new, promising medications have been introduced. Promising medications that are fast becoming first-line treatment, often in combination with methotrexate, are inhibitors of the anti-inflammatory protein tumor necrosis factor (TNF). These medicines include etanercept (Enbrel), infliximab (Remicade), and adalimumab (Humira), certolizumab (Cimzia), and golimumab (Simponi).
Other injectable biologic medications include anakinra (Kineret), which blocks the inflammatory protein interleukin-1, abatacept (Orencia), tocilizumab (Actemra), and rituximab) Rituxan. An oral biolotic is tofacitnib (Xeljanz)
Anti-inflammatory agents used to treat RA traditionally include aspirin and non-steroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen (Motrin, Advil), fenoprofen, indomethacin, naproxen (Naprosyn), and others.
These are widely used medications that are effective in relieving pain and inflammation associated with RA. However, the side effects associated with frequent use of many of these medications include life-threatening gastrointestinal bleeding and kidney damage.
A similar class of drugs, called COX-2 inhibitors, reduces the pain of arthritis without causing ulcer disease, and at least partially prevents the GI complaints associated with NSAIDs. Just one of these medicines, available by prescription only, is still on the market:
- Celecoxib (Celebrex)
Two other COX-2 inhibitors, valdecoxib (Bextra) and rofecoxib (Vioxx), are no longer available due to increased heart and stroke risks. Celebrex is also not without side effects and risks. Celecoxib may raise blood pressure, and long-term use might increase your risk for heart attack or stroke.
Antimalarial medications such as hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine) are also beneficial, usually in conjunction with methotrexate.
The benefits from these medications may take weeks or months to be apparent. Because they are associated with toxic side effects, frequent monitoring of blood tests while on these medications is imperative.
Other drugs that suppress the immune system, like azathioprine (Imuran) and cyclophosphamide (Cytoxan), are sometimes used in people who have failed other therapies. These medications, which are associated with toxic side effects, are usually reserved for severe cases of RA.
Corticosteroids have been used to reduce inflammation in RA for more than 40 years. However, because of potential long-term side effects, corticosteroid use is usually limited to short courses and low doses where possible. Side effects may include bruising, psychosis, thinning of the bones (osteoporosis), cataracts, weight gain, susceptibility to infections, diabetes, and high blood pressure. Several medications can be administered with steroids to minimize osteoporosis.
Consult a health care provider before long-term use of any medication, including over-the-counter medications.
Surgery
Occasionally, surgery is performed for severely affected joints. The most successful surgeries are those on the knees and hips. Usually, the first surgical treatment is removal of the synovium (synovectomy).
A later alternative is total joint replacement with a joint prosthesis. Surgeries can relieve joint pain, correct deformities, and modestly improve joint function. In extreme cases, total knee or hip replacement can mean the difference between being totally dependent on others and having an independent life at home.
Lifestyle changes
Adding omega-3 fats to your diet, such as EPA or DHA, may be helpful. Adding gamma-linolenic acid (GLA) to the diet may also be beneficial for people with RA.
Range-of-motion exercises and individualized exercise programs prescribed by a physical therapist can delay the loss of joint function.
Joint protection techniques, heat and cold treatments, and splints or orthotic devices to support and align joints may be very helpful.
Frequent rest periods between activities, as well as 8 to 10 hours of sleep per night, are recommended.
Other therapy
Sometimes therapists will use special machines to apply deep heat or electrical stimulation to reduce pain and improve joint mobility.
Occupational therapists can construct splints for your hand and wrist, and teach you how to best protect and use your joints when they are affected by arthritis. They also show people how to better cope with day-to-day tasks at work and at home, despite limitations caused by RA.
Monitoring
Depending on the medications being taken, regular blood or urine tests should be done to monitor both progress and negative side effects.
Reviewed By: Ariel D. Teitel, MD, MBA, Clinical Associate Professor of Medicine, Division of Rheumatology, NYU Langone Medical Center. Review provided by VeriMed Healthcare Network.
