Infertility in men - InDepth
Highlights
Causes of Male Infertility
Most cases of male infertility cases are due to low sperm counts, poor sperm quality, or both.
Sperm Abnormalities
Sperm abnormalities are a critical factor in male infertility. These abnormalities include:
- Low sperm count
- Poor sperm motility (movement)
- Abnormal sperm structure and shape
Risk Factors
Risk factors for male infertility include:
- Varicocele, an enlarged varicose vein in the spermatic cord that connects to the testicle, although whether a varicocele plays a role in male infertility is unclear.
- Aging, which can reduce sperm counts and motility and decrease the genetic quality of sperm
- Sexually transmitted infections, which can cause scarring in the male reproductive system or impair sperm function
- Lifestyle factors such as smoking and substance abuse
- Long-term or intensive exposure to certain types of chemicals, toxins, or medications
Diagnosis
In addition to a medical history and physical exam, specific tests for male infertility may include:
- Semen analysis to evaluate the quantity and quality of sperm
- Blood tests to evaluate hormone levels
- Imaging tests to look for structural problems
- Genetic testing to identify sperm DNA fragmentation, chromosomal defects, or genetic diseases
Treatment
Treatment for male infertility should first address any underlying medical conditions that may be contributing to fertility problems. Drug therapy may be used to treat hormonal disorders or infections. Surgery may be used to repair varicoceles in some men and correct any obstructions in the reproductive tract.
If fertility issues remain unresolved, intracytoplasmic sperm injection (ICSI) is commonly used in combination with in vitro fertilization (IVF) to achieve pregnancy when male infertility is a factor. ICSI involves injecting a single sperm into an egg obtained through IVF. The fertilized egg is then implanted back into the woman. Testicular sperm extraction (TESE) may sometimes be used to get viable sperm from the testes. TESE involves placing an anesthetic on the scrotum and passing a needle into the testicle to obtain some tissue. Sperm then can be found within this tissue. This sperm can sometimes be used for ICSI. Pregnancy success rates depend on many different factors.
Lifestyle Tips for Optimizing Fertility
The American Society for Reproductive Medicine recommends:
- A couple's best chance for conception is to have sex 2 to 3 times throughout a woman's cycle and every 1 to 2 days during a women's "fertile window" (the 6 days leading up to and including ovulation). Abstaining from sex for more than 5 to 10 days may adversely affect sperm health. But a couple's decision on how frequently to have sex is a personal choice.
- Avoid using water-based sexual lubricants as they can interfere with the sperm's ability to swim. Use instead canola oil, mineral oil, or commercial "fertility-friendly" labeled products.
- If you smoke, stop. Smoking may impair sperm quality, as can excessive alcohol use, recreational drugs, and anabolic steroids. It is also important to take care of your overall health including managing any long-term (chronic) health conditions such as high blood pressure and diabetes.
Introduction
Infertility is the failure of a couple to become pregnant after 1 year of regular, unprotected intercourse. However, fertility testing can be initiated before 1 year if the female partner is older than 35. About a third of infertility problems are due to male infertility, and another third are due to female infertility. In the remaining cases, infertility affects both partners or the cause is unclear.
Male infertility is due to problems with sperm or the structures associated with fertility.
The Male Reproductive System
The male reproductive system creates sperm cells that are produced in the seminiferous tubules within each testicle. The sperm have to reach the uterus and the fallopian tube in order to fertilize a woman's egg.
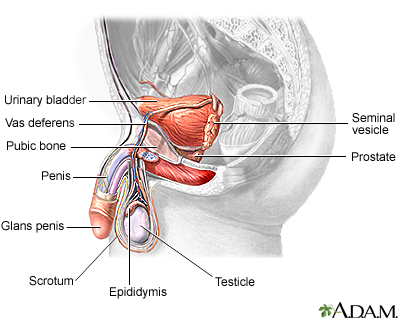
The male reproductive system includes the testicles, epididymis, vas deferens, seminal vesicles, prostate gland, urethra, and penis.
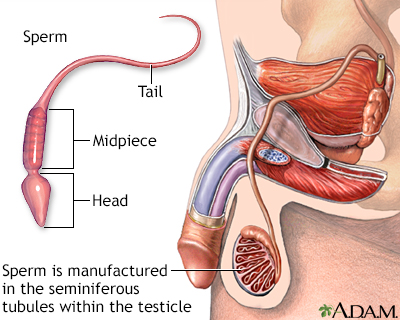
Sperm
Sperm are male reproductive cells. They are produced in the two testicles (testes). The testes are contained in the scrotal sac (scrotum).
Structure of Sperm
A mature sperm cell has three parts:
- The head consists of the nucleus, which is surrounded by the acrosome. The nucleus contains genetic material. The acrosome contains enzymes that penetrate the egg and allow the sperm to enter.
- The middle part contains mitochondria, which supply energy for the sperm to swim into the female genital tract.
- The tail of the sperm is the flagellum. The tail moves with whip-like movements back and forth to propel the sperm toward the egg.
Hormonal Regulation
Sperm production depends on three major hormones:
- Follicle-stimulating hormone (FSH) stimulates the production of sperm in the Sertoli cells, which are located inside the testicles' seminiferous tubules. The testicles contain hundreds of these microscopic tubules.
- Luteinizing hormone (LH) stimulates receptors in Leydig cells to produce testosterone. Leydig cells surround the seminiferous tubules.
- Testosterone is the most important male hormone.
FSH and LH are produced in the brain's pituitary gland. These hormones are also important for female reproduction. Testosterone is produced in the testicles.
Sperm Development
The scientific word for sperm development is spermatogenesis. This process begins in the testicle (testes):
- The testes are composed of coiled structures called seminiferous tubules, which are the sites of sperm production.
- Sperm are produced within nurturing Sertoli cells, which are located in the lower parts of the seminiferous tubules.
- Once sperm are produced, they pass through the seminiferous tubules and are collected in a structure of tightly coiled tubes called the epididymis. An epididymis lies along the back side of each testicle.
- Sperm mature in the epididymis and are stored there to await ejaculation.
Ejaculation
When a man experiences sexual excitement, his penis fills with blood and becomes erect. Nerves stimulate muscle contractions, which force the sperm out from the epididymis through the penis' urethra, where they are expelled:
- The sperm pass through the epididymis into a muscular tube called the vas deferens. The vas deferens connects the epididymis to the seminal vesicle and urethra.
- Muscle contractions in the vas deferens propel the sperm into the ampulla, where secretions from the seminal vesicle are added to form seminal fluid (semen). The seminal vesicles are sac-like glands attached to the vas deferens. They produce fructose, which provide energy for sperm movement.
- Each vas deferens and seminal vesicle join together to form an ejaculatory duct. The two ejaculatory ducts (left and right) converge into the prostate gland, which adds milky protein secretions to the seminal fluid.
- Semen is composed mainly of fluid from the seminal vesicles and the prostate gland. Sperm make up only a small percentage of semen.
- The ejaculatory ducts open into the urethra. The urethra is the same channel in the penis through which a man urinates. During orgasm, muscles close the bladder neck so that urine cannot enter the urethra and the semen cannot enter the bladder.
- The semen is forced through the urethra during ejaculation, the final stage of orgasm when the sperm is literally ejected from the penis.
- A man's ejaculate contains over 100 million sperm. Only 1 sperm fertilizes the egg.
Causes
Most cases of male infertility cases are due to low sperm counts, poor sperm quality, or both. The remaining cases of male infertility are caused by a variety of factors including anatomical problems, hormonal imbalances, and genetic defects.
Sperm Abnormalities
Sperm abnormalities can be caused by many factors. They include congenital birth defects, disease, chemical exposure, and lifestyle habits. In many cases, the causes of sperm abnormalities are unknown.
Sperm abnormalities are categorized by whether they affect sperm count, sperm movement, or sperm shape:
Low Sperm Count (Oligospermia).
A sperm count of less than 20 million/mL is considered low sperm.Azoospermia
is the complete absence of sperm cells in the ejaculate. Obstructions in the vas deferens (such as from vasectomy) or other areas can block the passage of sperm and reduce sperm counts.Poor Sperm Motility (Asthenospermia).
Sperm motility is the sperm's ability to move. If movement is slow or not in a straight line, the sperm have difficulty invading the cervical mucus or penetrating the hard outer shell of the egg. Sperm that move sluggishly may have genetic or other defects that render them incapable of fertilizing the egg. Poor sperm motility may be associated with DNA fragmentation (damage) and may increase the risk for passing on genetic diseases.Abnormal Sperm Morphology (Teratospermia).
Morphology refers to shape and structure. Abnormally shaped sperm cannot fertilize an egg. The perfect sperm structure is an oval head and long tail.
Retrograde Ejaculation
Retrograde ejaculation occurs when the muscles of the bladder wall do not function properly during orgasm and sperm are forced backward into the bladder instead of forward out of the urethra. Sperm number and quality are often impaired.
Retrograde ejaculation can result from several conditions:
- Surgery to the lower part of the bladder or prostate (the most common cause of retrograde ejaculation)
- Nerve damage caused by spinal cord injury or surgery, or diseases such as diabetes and multiple sclerosis
- Medications such as alpha blockers used to treat prostate gland enlargement
Anatomical Abnormalities
Any anatomical abnormalities that damage or block the testes, tubes, or other reproductive structures can affect sperm and reduce fertility. These conditions are often birth defects such as:
Cryptorchidism
(undescended testes) is a condition in which the testicles fail to descend from the abdomen into the scrotum.Hypospadias
is a condition in which the urinary opening is on the underside of the penis.- Blockages or other problems in the epididymis or ejaculatory ducts are also birth defects. Some men are born lacking the vas deferens, the tube that carries sperm from the testicles.
Hormonal Deficiencies
Any condition that affects the production of the hormones testosterone, FSH, or LH can affect sperm production:
- Low levels of FSH and LH can be caused by pituitary gland tumors or other problems in the pituitary or hypothalamus
- Testosterone deficiency (hypogonadism) can result from genetic disorders, thyroid disorders, medications, or cancer treatments
Antisperm Antibodies
Sometimes a man's immune system mistakenly identifies sperm as a foreign invader and produces antibodies that attack and destroy the sperm. Antisperm antibodies may result from surgery, infections, or trauma or twisting of the testicles.
Genetic Disorders
Certain inherited disorders can impair fertility. Examples include:
- Cystic fibrosis can cause missing or obstructed vas deferens.
- Klinefelter syndrome results when a man has one or more extra X chromosomes. It causes low testosterone levels and abnormalities of the seminiferous tubules
- Kartagener syndrome causes problems with sperm motility.
- Y chromosome microdeletion can result in loss of genes that are important for sperm formation. A significant proportion of men with azoospermia and oligospermia also have Y chromosome microdeletions.
There is continued research into genetic causes or risk factors for male infertility. However, genetic testing as part of an evaluation appears to be in the research stages at this time.
Risk Factors
Varicocele
A varicocele is an abnormally enlarged and twisted (varicose) vein in the spermatic cord that connects to the testicle. Varicoceles are found more often in men who report infertility problems. However, most men with a varicocele are fertile. It is not clear how much they affect fertility or by what mechanisms. They can raise testicular temperature, which may have effects on sperm production, movement, and shape.
Age
Age-related sperm changes in men are not abrupt, but are a gradual process. Aging can adversely affect sperm counts and sperm motility (the sperm's ability to swim quickly and move in a straight line). The genetic quality of sperm declines as a man ages.
Medical Conditions
Medical conditions that can affect male fertility include:
- Sexually transmitted infections, such as gonorrhea, chlamydia, and human papillomaviruses
- Infections in the prostate gland, testicles, or urethra
- Surgery or injury to the testicles
- Uncontrolled high blood pressure or diabetes
- Obesity
- Thyroid disorders
- Certain types of drugs such as testosterone replacement therapy and anabolic steroids (current or previous use).
- Chemotherapy and radiation cancer treatments
Lifestyle Factors
A number of lifestyle factors may affect sperm and contribute to infertility. They include:
- Cigarette smoking
- Drug abuse with cocaine, opioids, or marijuana
- Prolonged bicycling or horseback riding
- Excessive exercise
- Hot tubs and saunas
- Emotional stress
Environmental Factors
Occupational or other long-term exposure to certain types of toxins and chemicals (such as herbicides and pesticides) may reduce sperm count by either affecting testicular function or altering hormone systems. Estrogen-like and hormone-disrupting chemicals such as bisphenol A, phthalates, and organochlorines are particular concerns.
Long-term (chronic) exposure to heavy metals such as lead, cadmium, or arsenic may affect sperm quality. These chemicals usually affect men who have long-term and intense occupational exposure to them.
Diagnosis
Health care providers recommend that both male and female partners get tested for infertility if pregnancy fails to occur after 1 year of regular unprotected sexual intercourse. Fertility testing should be done earlier if a woman is over age 35 or if either partner has known risk factors for infertility. If an evaluation of both male and female partners is possible, semen analysis should be done before more invasive testing of the female partner.
Because male infertility can be due to many different conditions, a number of tests are used for diagnosis. Your provider may refer you to a fertility specialist, usually a urologist, for specific tests.
Medical History
The provider will ask about any medical or sexual factors that might affect fertility, such as:
- Frequency and timing of sexual intercourse
- Duration of infertility and any prior problems with fertility
- Childhood illnesses and any problems in development
- Any recent or current illnesses (such as diabetes, respiratory infections, allergies, or cancer)
- Sexual history, including any sexually transmitted infections
- Any exposure to toxins, such as chemicals or radiation
- History of surgeries or trauma to the genital area
- Medication use
- Alcohol, tobacco, anabolic steroid, or recreational drug use
- Any family history of reproductive problems
Physical Exam
The provider will carefully examine the scrotum and testicles. Varicoceles can be felt during examination of the scrotum. (They are described as feeling like "a bag of worms.") The doctor may also check the prostate gland. The provider will examine the penis for any signs of infection or anatomical abnormalities.
Semen Analysis
The basic test to evaluate a man's fertility is a semen analysis. The sperm collection involves the following steps:
- Abstain from ejaculation for several days before (but no more than 5 days) the test because each ejaculation can reduce sperm count.
- Collect a sample of your semen either by masturbating into a sterilized cup or having sexual intercourse using a special collection condom.
- Keep the sample at room or body temperature and deliver it promptly to the laboratory or medical office. The sperm should be analyzed within 1 hour of collection.
- Because sperm counts can fluctuate, collection and analysis may need to be repeated over several months.
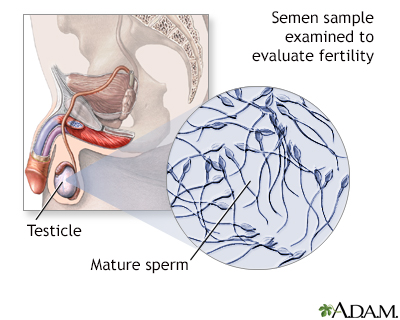
The sperm count test is performed if a man's fertility is in question. It is helpful in determining if there is a problem in sperm production or quality of the sperm as a cause of infertility. The test may also be used after a vasectomy to make sure there are no sperm in the semen.
A semen analysis will provide information on:
- Amount of semen produced (volume)
- Number of sperm per milliliter of semen (concentration)
- Total number of sperm in the sample (count)
- Percent of live sperm (viability)
- Percentage of moving sperm (motility)
- Shape of sperm (morphology)
Semen Volume
The amount of semen is important. Most men ejaculate between 2.5 to 5 milliliters of semen. Either significantly high or low amounts can indicate problems. Low amounts (less than 1.5 milliliters) are a sign of fewer sperm. High amounts may dilute the concentration of sperm.
Semen Concentration
Concentration refers to the amount of sperm found in 1 milliliter of semen. A normal concentration is at least 20 million sperm per milliliter.
Sperm Count
Sperm count refers to the number of sperm found in the entire sample of semen. In general, a normal sperm count is considered to be at least 40 million.
Sperm Viability
At least 50% of the sperm in the semen sample should be alive (viable).
Sperm Motility
Motility (the speed and quality of movement) is graded on a scale from 0 (worst) to 4 (best). Grades 3 and 4 indicate good mobility. At least 40% of the sperm should be motile.
Sperm Morphology
Morphology is the size, shape, and structure of the sperm. At least 50% of the sperm should be of normal appearance.
Other Factors
The acidity of the semen is tested (pH should be 7.2 or greater). The lab will test for presence or absence of certain chemicals and enzymes, such as fructose. The semen will be tested for how thick it is and how quickly it liquefies, and whether it clumps together.
Other Sperm Tests
Although less commonly performed, sperm penetration tests may be used to evaluate function. For example, the sperm penetration assay measure the sperm's ability to penetrate specially prepared hamster eggs. The exact role of these tests for most people with infertility remains unclear.
A laboratory sperm-cervical mucus test (Kurzrock-Miller or Kremer test) may also be used to evaluate how well sperm move in cervical mucus. Either the female partner's mucus or donated midcycle mucus can be used in this test.
Laboratory Tests
Blood tests may be used to check for hormone levels of testosterone, FSH, and LH. A blood test can also check for evidence of sexually transmitted infections.
A post-ejaculatory urine sample can detect presence of sperm, which may indicate retrograde ejaculation.
Imaging Tests
Ultrasound uses sound waves to produce an image. Ultrasound imaging may be used to check for abnormalities or blockages in the testicles, or to find varicoceles that are too small for physical detection.
In transrectal ultrasound, a probe is inserted into the rectum to provide images of the prostate gland, vas deferens, and seminal vesicles.
Testicular Biopsy
A small tissue sample of the testicle may be taken using a thin needle. A biopsy may be performed for diagnostic purposes to evaluate sperm production function. A biopsy may also be used to collect sperm that will be used in an intracytoplasmic sperm injection (ICSI) fertility procedure.
Genetic Testing
Genetic testing may be recommended for some men, particularly those who will use ICSI. Genetic testing can help identify sperm DNA fragmentation, chromosomal defects, or the possibility of genetic diseases that can be passed on to children.
Treatment
Treatment for male infertility depends on the cause of infertility, and whether a cause is found. Treatments may include:
- Drug therapy to treat hormone imbalances or infections.
- Surgery to repair varicoceles and correct any obstructions in the reproductive tract. However, there is some controversy over whether varicocele treatment actually improves fertility or the chance for conception.
- Fertility treatments with testicular sperm extraction (TESE), intrauterine insemination (IUI), or ICSI.
Drug Therapy
Antioxidants are man-made or natural substances that may prevent or delay some types of cell damage. There is some thought that these agents may improve sperm function and therefore fertility.
- Common antioxidants include carnitine, lycopene, glutathione, vitamins E, C, and A.
- They are found in many foods, such as fruits and vegetables. They may also be found as dietary supplements.
- The evidence that these substances improve pregnancy rates is poor.
Endocrine treatments may be tried in selected men with identified endocrine dysfunction as a possible cause. The goal of these treatments is to increase the level of testosterone within the testes. These include:
- Clomiphene and tamoxifen
- Aromatase inhibitors
Varicocelectomy (Varicocele Removal)
Conditions for treating a varicocele that can be felt on physical exam include both of the following:
- Female partner has either normal fertility or has a fertility problem that can be treated.
- Abnormal semen findings with analysis.
Depending on semen analysis findings, other fertility treatments such as IUI, IVF, or ICSI are other options before surgical treatment of the varicocele.
Invasive varicocele treatment options include:
- A surgical approach, most often through the inguinal area.
- A percutaneous (through the skin) approach injecting an agent or device into the widened vein which feeds the varicocele to obstruct it.
In general, surgical invasive treatment of varicoceles has been found to increase sperm counts by around 12 million and improve sperm motility by around 10%. These improvements take 3 to 6 months to be evident.
Studies that report on pregnancy rates after treatment appeared to indicate an improvement for couples with otherwise unexplained infertility. The quality of these studies is generally not considered to be high.
Choosing a Fertility Clinic
IUI, ICSI, and other assisted reproductive technologies (ART) are offered by fertility clinics. ICSI is used in combination with IVF. Choosing a good fertility clinic is important. Fertility procedures are expensive and often not covered by insurance.
You and your partner should ask the fertility clinic questions about:
- The live-birth success rate, not just pregnancy success rate. (Multiple births, such as twins or triplets, are counted as one live birth.)
- The qualifications and training of the fertility specialists.
- What treatments are available.
- How your age or your partner's age may affect the choice of treatment.
- Whether your treatments will be covered by insurance.
Special Considerations for Patients with Cancer
Adolescents and adult men undergoing cancer treatments who may want to father children in the future should consider banking and freezing their sperm for later use in assisted reproductive therapies. This technique is called sperm cryopreservation.
Sperm cryopreservation is recommended by the American Society of Clinical Oncology as the method with the highest likelihood of success for male cancer survivors. It can be easily done and will not delay cancer treatment.
These banking methods are not appropriate for pre-adolescent boys being treated for childhood cancers such as leukemia. Researchers are investigating ways that stem cell transplantation may someday help these children regain their fertility while avoiding leukemia relapse.
Assisted Reproductive Technologies
Assisted reproductive technologies (ART) are medical techniques that help couples conceive. These procedures involve either:
- A couple's own eggs or sperm
- Donor eggs, sperm, or embryos
Fertilization may occur either in the laboratory or in the uterus. In the United States, the number of live birth deliveries from ART has doubled in the last decade. About 70,000 live births (deliveries of one or more infants) occur each year using ART. According to the Centers for Disease Control (CDC), around 1.7% of all babies born in the United States every year are conceived using ART.
Technically, the term ART refers only to fertility treatments, such as IVF and its variants, which handle both egg and sperm. Therefore, IUI or artificial insemination is not officially considered a form of ART.
Sperm Retrieval
Before fertilization using IUI or ICSI can take place, the sperm must be collected and prepared.
When a man has no available sperm in the ejaculate (usually from blockage, vasectomy, or lack of vas deferens), the sperm must be retrieved from the testes or the epididymis.
Various microsurgical techniques are used for retrieval. The procedure may be done under local or general anesthesia, using a spring-loaded biopsy device, a thin needle, incisions, or microsurgical techniques. These are forms of TESE. Most procedures can be done on an outpatient basis, and the man returns home the same day.
Sperm Washing
Sperm washing is done to prepare the sperm for use in ART procedures. Sperm washing can help remove chemicals (prostaglandins) that can cause the woman's uterus to contract and cramp. Sperm washing can also help remove sexually transmitted viruses, such as HIV and hepatitis, which could potentially be transmitted to the woman during fertility treatment.
There are three basic methods for sperm washing:
- Simple sperm wash dilutes sperm in a test tube and then uses a centrifuge to retrieve sperm cells.
- Density gradient sperm wash is similar to the simple sperm wash but is better for separating dead sperm from live, healthy sperm cells.
- Swim-up technique does not use a centrifuge. Instead, it uses a culture dish with a medium that attracts sperm powerful enough to swim up to the nutrient mixture. This technique is useful for harvesting healthy sperm with good motility.
Freezing Sperm
Sperm can be fresh or it can be frozen in advance. Men who have no sperm count not caused by obstruction (nonobstructive azoospermia) often use frozen sperm. Sperm that will be frozen is retrieved using a testicular biopsy. Evidence indicates that both fresh and frozen sperm work equally well for fertilization outcomes.
Intrauterine Insemination (Artificial Insemination)
Artificial insemination (AI) is the least complex of fertility procedures and is often tried first in uncomplicated cases of infertility. AI involves placing the sperm directly in the cervix (called intracervical insemination) or into the uterus (called intrauterine insemination, or IUI). IUI is the standard AI procedure.
IUI may be used under the following circumstances:
- If the man's sperm count is very low
- If there is decreased sperm motility
- If the woman has cervical scarring
- When unexplained infertility exists in both partners
- When donor sperm are required
The IUI procedure is as follows:
- A woman usually takes fertility drugs in advance to stimulate egg production.
- The man must produce sperm at the time the woman is ovulating.
- The sperm are washed and then inserted into the uterine cavity through a long, thin catheter.
The administration of fertility drugs and sperm retrieval is timed so that the process can coincide with time of ovulation.
If a woman fails to conceive after IUI, she may be a candidate for IVF.
Intracytoplasmic Sperm Injection (ICSI)
ICSI is an ART used for couples when male infertility is the main factor. It is used in combination with IVF. It involves injecting a single sperm into an egg obtained from IVF.
In the ICSI procedure:
- A tiny glass tube (called a holding pipet) stabilizes the egg.
- A second glass tube (called the injection pipet) is used to penetrate the egg's membrane and deposit a single sperm into the egg.
- The egg is released into a drop of cultured medium.
- If fertilized, the egg is allowed to develop for 1 to 2 days and then is either frozen or implanted.
The greatest concern with this procedure has been whether it increases the risk for birth defects. Many, but not all, studies have reported no higher risks of birth defects in children born using ICSI procedures. However, if the father's infertility was due to genetic issues, this genetic defect may be passed on to male children conceived through ICSI. Recent studies suggest that fetuses conceived with ICSI and IVF may have a higher risk of congenital heart defects.
Because several embryos are implanted to increase the chances for pregnancy success, multiple births can occur with IVF/ICSI. Multiple pregnancies increase the risks for a mother and her babies. In particular, there is increased risk for premature delivery and low birth weight.
IVF/ICSI can also pose specific risks for the woman. These risks include ovarian hyperstimulation syndrome, a condition induced by the fertility drugs used in the procedure. Ovarian hyperstimulation can result in dangerous fluid and electrolyte imbalances as well as increased blood pressure and higher risk for blood clots.
Another concern has been whether the ICSI procedure is overused. Some providers recommend ICSI for women who have failed prior IVF attempts or who have few or poor-quality eggs, even if their male partners have normal semen measurements. According to the Society for Assisted Reproductive Technology, there is little evidence that ICSI helps improve pregnancy success for couples who do not have a problem with male factor infertility.
Success Rates
Not all IVF/ICSI cycles result in pregnancy, and not all IVF-achieved pregnancies result in live births. When the woman's own eggs are used, results are better with fresh embryos than frozen embryos. Success rates provided by fertility clinics are not always a reliable indicator as they depend on many variables, including the age of the patients. The chances for success are best for women younger than age 37.
Lifestyle Changes
Planning Sexual Activity
The Fertile Window
Couples can optimize their chances for conception by planning sexual intercourse during the woman's fertile window:
- The "fertile window" is 6 days long, starts 5 days before a woman's ovulation, and ends the day of ovulation. (Ovulation is when an egg is released to await fertilization. The egg lives only 12 to 24 hours after ovulation and must be fertilized by a sperm during this time in order for pregnancy to occur.)
- In a woman with a 28-day menstrual cycle, ovulation usually occurs around day 14 (14 days after the start of her menstrual period), which means the fertile window occurs from days 9 to 14. However, the length of menstrual cycles, and fertile windows, vary from woman to woman.
- The chance that intercourse will result in pregnancy is highest during the fertile window, during the 3-day interval that ends on the day of ovulation.
Frequency of Intercourse
Evidence indicates that chances are best for conception when sexual intercourse occurs every 1 to 2 days, during the fertile window. Less frequent regular sexual intercourse (2 to 3 times a week) also achieves good results. However, couples need to make their own personal choices about what amount of sexual activity is appropriate, comfortable, and desirable. Data suggest that abstinence (not having sex) for more than 5 to 10 days may adversely affect sperm health.
Sexual Practices
There is no evidence that any particular sexual positions, or resting after sex, help increase the chances for pregnancy. There is also no evidence that whether or not a woman achieves orgasm affects the likelihood of her becoming pregnant. Couples should be aware that water-based sexual lubricants (Astroglide, KY Jelly, saliva) can damage sperm's ability to swim and should not be used. For lubrication, try mineral oil, canola oil, or commercially available "fertility-friendly" products such as Pre-Seed, which do not harm sperm.
Fertility and Seasonal Changes
Some studies have reported higher sperm counts and better motility in the winter than in the summer.
Dietary Considerations
Everyone should eat a healthy diet rich in fresh fruits, vegetables, and whole grains. Replace animal fats with monounsaturated oils, such as olive oil. Certain specific nutrients and vitamins have been studied for their effects on male infertility and sperm health. They include antioxidant vitamins (vitamin C, vitamin E) and the dietary supplements L-carnitine and L-acetylcarnitine. To date, there is no conclusive evidence that they are effective.
Other Lifestyle Changes
Other tips for helping fertility include:
- Control any long-term (chronic) medical conditions you may have such as high blood pressure and diabetes.
- Overweight men should try to reduce their weight as obesity may be associated with infertility. However, good clinical studies to support an improvement in fertility have not been done.
- Avoid cigarettes and any drugs that may affect sperm count or reduce sexual function.
- Get sufficient rest and exercise moderately but regularly. (Excessive exercise may impair fertility.)
- Although there is no conclusive evidence that tight underwear or pants pose a threat to male fertility, there is no harm in wearing looser clothing (in other words, choose boxers over briefs).
- To prevent overheating of the testes, men should avoid hot baths, prolonged showers, and steam rooms. Similarly, avoid using a laptop on your lap for long periods of time.
- Stress may affect hormones that contribute to sperm quality. It is not known if stress reduction techniques can improve fertility, but they may help couples endure the difficult processes involved in fertility treatments.
Dealing with Stress
The fertility treatment process presents a roller coaster of emotions. There are almost no sure ways to predict which couples will eventually conceive. Some couples with multiple problems will overcome great odds, while other, seemingly fertile, couples fail to conceive. Many of the new treatments are remarkable, but a live birth is never guaranteed. The emotional burden on the couple is considerable, and some planning is helpful:
- Decide in advance how many and what kind of procedures will be emotionally and financially acceptable and attempt to determine a final limit. Fertility treatments can be expensive. A successful pregnancy often depends on repeated attempts.
- Prepare for multiple births as a possible outcome for successful pregnancy (if an ART is used). A pregnancy that results in a multiple birth introduces new complexities and emotional problems.
- Determine alternatives (adoption, donor sperm or egg, or having no children) as early as possible in the fertility process. This can reduce anxiety during treatments and feelings of disappointment if conception does not occur.
Resources
- American Society for Reproductive Medicine -- www.asrm.org
- Urology Care Foundation -- www.urologyhealth.org
- Path to Parenthood -- www.path2parenthood.org
- Society for Assisted Reproductive Technology -- www.sart.org
- Centers for Disease Control and Prevention: Assisted Reproductive Technology (ART) -- www.cdc.gov/art/index.html
References
American Urological Association. The optimal evaluation of the infertile male. AUA best practice statement. www.auanet.org/documents//education/clinical-guidance/Male-Infertility-d.pdf. Updated 2010. Accessed February 27, 2020.
Barak S, Baker HWG. Clinical management of male infertility. In: Jameson JL, De Groot LJ, de Kretser DM, et al, eds. Endocrinology: Adult and Pediatric. 7th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 141.
Centers for Disease Control and Prevention website. ART success rates. www.cdc.gov/art/artdata/index.html. Updated November 15, 2019. Accessed January 28, 2020.
Ferlin A, Foresta C. New genetic markers for male infertility. Curr Opin Obstet Gynecol. 2014;26(3):193-198. PMID: 24743183 pubmed.ncbi.nlm.nih.gov/24743183.
Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services: recommendations of CDC and the US Office of Population Affairs. MMWR Recomm Rep. 2014;63(RR-04):1-54. PMID: 24759690 pubmed.ncbi.nlm.nih.gov/24759690.
Giorgione V, Parazzini F, Fesslova V, et al. Congenital heart defects in IVF/ICSI pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(1):33-42. PMID: 29164811 pubmed.ncbi.nlm.nih.gov/29164811.
Hornstein MD. State of the ART: assisted reproductive technologies in the United States. Reprod Sci. 2016;23(12):1630-1633. PMID: 27624310 pubmed.ncbi.nlm.nih.gov/27624310.
Hotaling JM, Patel Z. Male endocrine dysfunction. Urol Clin North Am. 2014;41(1):39-53. PMID: 24286766 pubmed.ncbi.nlm.nih.gov/24286766.
Krausz C, Casamonti E. Spermatogenic failure and the Y chromosome. Hum Genet. 2017;136(5):637-655. PMID: 28456834 pubmed.ncbi.nlm.nih.gov/28456834.
Lindsay TJ, Vitrikas KR. Evaluation and treatment of infertility. Am Fam Physician. 2015;91(5):308-314. PMID: 25822387 pubmed.ncbi.nlm.nih.gov/25822387.
Matsumoto AM, Anawait BD. Testicular disorders. In: Jameson JL, De Groot LJ, de Kretser DM, et al, eds. Endocrinology: Adult and Pediatric. 7th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 19.
Medrano JV, Andrés MDM, García S, et al. Basic and clinical approaches for fertility preservation and restoration in cancer patients. Trends Biotechnol. 2018;36(2):199-215. PMID: 29153762 pubmed.ncbi.nlm.nih.gov/29153762.
Niederberger CS, Ohlander SJ, Pagani RL. Male infertility. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 66.
Oehninger S, Franken DR, Ombelet W. Sperm functional tests. Fertil Steril. 2014;102(6):1528-1533. PMID: 25450304 pubmed.ncbi.nlm.nih.gov/25450304.
Practice Committee of the American Society for Reproductive Medicine in Collaboration With the Society for Male Reproduction and Urology. Diagnostic evaluation of sexual dysfunction in the male partner in the setting of infertility: a committee opinion. Fertil Steril. 2018;110(5):833-837. doi: 10.1016/j.fertnstert.2018.07.010. PMID: 30316420 pubmed.ncbi.nlm.nih.gov/30316420.
Practice Committee of American Society for Reproductive Medicine in collaboration with Society for Reproductive Endocrinology and Infertility. Optimizing natural fertility: a committee opinion. Fertil Steril. 2013;100(3):631-637. PMID: 23993665 pubmed.ncbi.nlm.nih.gov/23993665.
Practice Committees of the American Society for Reproductive Medicine and Society for Assisted Reproductive Technology. Intracytoplasmic sperm injection (ICSI) for non-male factor infertility: a committee opinion. Fertil Steril. 2012;98(6):1395-1399. PMID: 22981171 pubmed.ncbi.nlm.nih.gov/22981171.
Practice Committee of the American Society for Reproductive Medicine; Society for Male Reproduction and Urology. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2014;102(6):1556-1560. PMID: 25458620 pubmed.ncbi.nlm.nih.gov/25458620.
Practice Committee of the American Society for Reproductive Medicine in collaboration with the Society for Male Reproduction and Urology. The management of obstructive azoospermia: a committee opinion. Fertil Steril. 2019;111(5):873–880. PMID: 31029241 pubmed.ncbi.nlm.nih.gov/31029241.
Practice Committee of the American Society for Reproductive Medicine. Management of nonobstructive azoospermia: a committee opinion. Fertil Steril. 2018;110(7):1239–1245. PMID: 30503112 pubmed.ncbi.nlm.nih.gov/30503112.
Practice Committee of the American Society for Reproductive Medicine. Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil Steril. 2018;110(4):611–618. PMID: 30196946 pubmed.ncbi.nlm.nih.gov/30196946.
Showell MG, Mackenzie-Proctor R, Brown J, Yazdani A, Stankiewicz MT, Hart RJ. Antioxidants for male subfertility. Cochrane Database Syst Rev. 2014;12:CD007411. PMID: 25504418 pubmed.ncbi.nlm.nih.gov/25504418.
Tatem AJ, Brannigan RE. The role of microsurgical varicocelectomy in treating male infertility. Transl Androl Urol. 2017;6(4):722-729. PMID: 28904905 pubmed.ncbi.nlm.nih.gov/28904905.
Thurston L, Abbara A, Dhillo WS. Investigation and management of subfertility. J Clin Pathol. 2019;72(9):579-587. PMID: 31296604 pubmed.ncbi.nlm.nih.gov/31296604.
|
Review Date:
2/27/2020 Reviewed By: Sovrin M. Shah, MD, Assistant Professor, Department of Urology, The Icahn School of Medicine at Mount Sinai, New York, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. |







