Pregnancy SmartSiteTM
Choking - unconscious adult or child over 1 year; First aid - choking - unconscious adult or child over 1 year; CPR - choking - unconscious adult or child over 1 year DefinitionChoking is when someone is having a very hard time breathing because food, a toy, or other object is blocking the throat or windpipe (airway). A choking person's airway may be blocked so that not enough oxygen reaches the lungs. Without oxygen, brain damage can occur in as little as 4 minutes. Rapid first aid for choking can save a person's life. This article discusses choking in adults or children over age 1 year who have lost alertness (are unconscious). CausesChoking may be caused by:
SymptomsSymptoms of choking when a person is unconscious include:
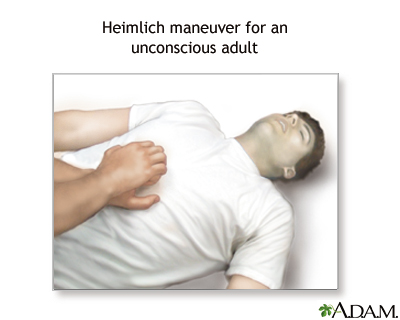
First AidTell someone to call 911 or the local emergency number while you begin first aid and CPR. If you are alone, shout for help and begin first aid and CPR.
If the person starts having seizures (convulsions), give first aid for this problem. After removing the object that caused the choking, keep the person still and get medical help. Anyone who is choking should have a medical examination. This is because the person can have complications not only from the choking, but also from the first aid measures that were taken. Do NotDo not try to grasp an object that is lodged in the person's throat. This may push it farther down the airway. If you can see the object in the mouth, it may be removed. When to Contact a Medical ProfessionalSeek medical help right away if someone is found unconscious. In the days following a choking episode, contact a health care provider right away if the person develops:
The above signs may indicate:
PreventionTo prevent choking:
ReferencesDuff JP, Topjian AA, Berg MD, et al. 2019 American Heart Association focused update on pediatric basic life support: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2020;145(1):e20191358. PMID: 31727861 pubmed.ncbi.nlm.nih.gov/31727861/. Easter JS. Pediatric resuscitation. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 158. Goodloe JM, Soulek J. Foreign bodies. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 51. Haas NL, Kurz MC. Adult resuscitation. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 5. Hewett Brumberg EK, Douma MJ, Alibertis K, et al. American Heart Association and American Red Cross. 2024 American Heart Association and American Red Cross guidelines for first aid. Circulation. 2024;150(24):e519-e579. PMID: 39540278 pubmed.ncbi.nlm.nih.gov/39540278/. Perman SM, Elmer J, Maciel CB, et al. 2023 American Heart Association focused update on adult advanced cardiovascular life support: An update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2023;149(5):e254-e273. PMID: 38108133 pubmed.ncbi.nlm.nih.gov/38108133/. Rose E. Pediatric upper airway obstruction and infections. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 162. | ||
| ||
Review Date: 1/8/2025 Reviewed By: Jesse Borke, MD, CPE, FAAEM, FACEP, Attending Physician at Kaiser Permanente, Orange County, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 First Aid for Chok...
First Aid for Chok...
