Pregnancy SmartSiteTM
Blood loss; Open injury bleeding DefinitionBleeding is the loss of blood. Bleeding may be:
Bleeding may occur:
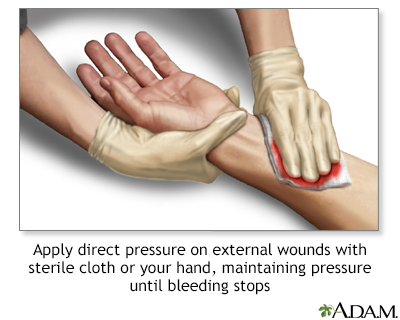
ConsiderationsGet emergency medical help for severe bleeding. This is very important if you think there is internal bleeding. Internal bleeding can very quickly become life threatening. Immediate medical care is needed. Serious injuries may cause heavy bleeding. Sometimes, minor injuries can bleed a lot. An example is a scalp wound. You may bleed a lot if you take blood-thinning medicine or have a bleeding disorder such as hemophilia. Bleeding in such people requires medical attention right away. The most important step for external bleeding is to apply direct pressure. This will likely stop most external bleeding. Always wash your hands before (if possible) and after giving first aid to someone who is bleeding. This helps prevent infection. Try to use latex gloves when treating someone who is bleeding. Latex gloves should be in every first aid kit. People allergic to latex can use nonlatex gloves. You can catch infections, such as viral hepatitis or HIV/AIDS, if you touch infected blood and it gets into an open wound, even a small one. Although puncture wounds usually don't bleed very much, they carry a higher risk for infection. Seek medical care to prevent tetanus or other infection. Abdominal, pelvic, groin, neck, and chest wounds can be very serious because of the possibility of severe internal bleeding. They may not look very serious, but can result in shock and death.
Blood loss can cause blood to collect under the skin, turning it black and blue (bruised). Apply a cool compress to the area as soon as possible to reduce swelling. Do not place ice directly on the skin. Wrap the ice in a towel first. CausesBleeding can be caused by injuries, or it can be spontaneous. Spontaneous bleeding most commonly occurs with problems in the joints, or gastrointestinal or urogenital tracts. SymptomsYou may have symptoms such as:
Bleeding can also cause shock, which may include any of the following symptoms:
Symptoms of internal bleeding may include those listed above for shock as well as the following:
Blood coming from a natural opening in the body may also be a sign of internal bleeding. These symptoms include:
First AidFirst aid is appropriate for external bleeding. If bleeding is severe, or if you think there is internal bleeding, or the person is in shock, get emergency help.
WHEN TO USE A TOURNIQUET If continuous pressure has not stopped the bleeding, and bleeding is extremely severe (life threatening), a tourniquet can be used until medical help arrives.
Do NotDo not peek at a wound to see if the bleeding is stopping. The less a wound is disturbed, the more likely it is that you will be able to control the bleeding. Do not probe a wound or pull out any embedded object from a wound. This will usually cause more bleeding and harm. Do not remove a dressing if it becomes soaked with blood. Instead, add a new one on top. Do not try to clean a large wound. This can cause heavier bleeding. Do not try to clean a wound after you get the bleeding under control. Get medical help. When to Contact a Medical ProfessionalSeek medical help right away if:
PreventionUse good judgment and keep knives and sharp objects away from small children. Stay up-to-date on vaccinations. ReferencesBulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):163-173. PMID: 24641269 pubmed.ncbi.nlm.nih.gov/24641269. Hayward CPM, Ma AD. Evaluation of the patient with suspected bleeding disorders. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 126. Qasim Z. Prehospital management of the trauma patient. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:1224-1230. Simon BC, Hern HG. Wound management principles. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 50. | ||
| ||
Review Date: 11/2/2023 Reviewed By: Jesse Borke, MD, CPE, FAAEM, FACEP, Attending Physician at Kaiser Permanente, Orange County, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. View References The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | ||


 Stopping bleeding ...
Stopping bleeding ...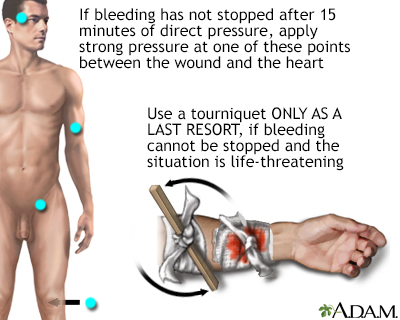 Stopping bleeding ...
Stopping bleeding ...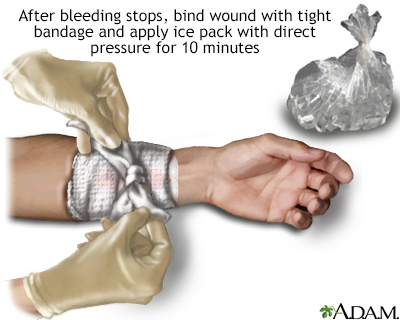 Stopping bleeding ...
Stopping bleeding ...
